Top 12 Medical Technology Tools Used by US Clinics in 2026

Riten Debnath
17 Jan, 2026

As we move through 2026, the physical equipment inside an American medical clinic has undergone a quiet but radical transformation. The traditional tools we’ve known for decadesthe heavy ultrasound cart, the analog stethoscope, and the manual blood pressure cuff, are being replaced by handheld, AI-integrated, and cloud-connected devices that bring hospital-grade diagnostics directly to the point of care. These tools are not just "gadgets"; they are critical assets that allow smaller clinics to perform complex screenings that previously required a trip to a major imaging center. By digitizing the physical exam, these technologies are reducing wait times, improving diagnostic accuracy, and allowing clinicians to spend more time looking at their patients rather than at their screens.
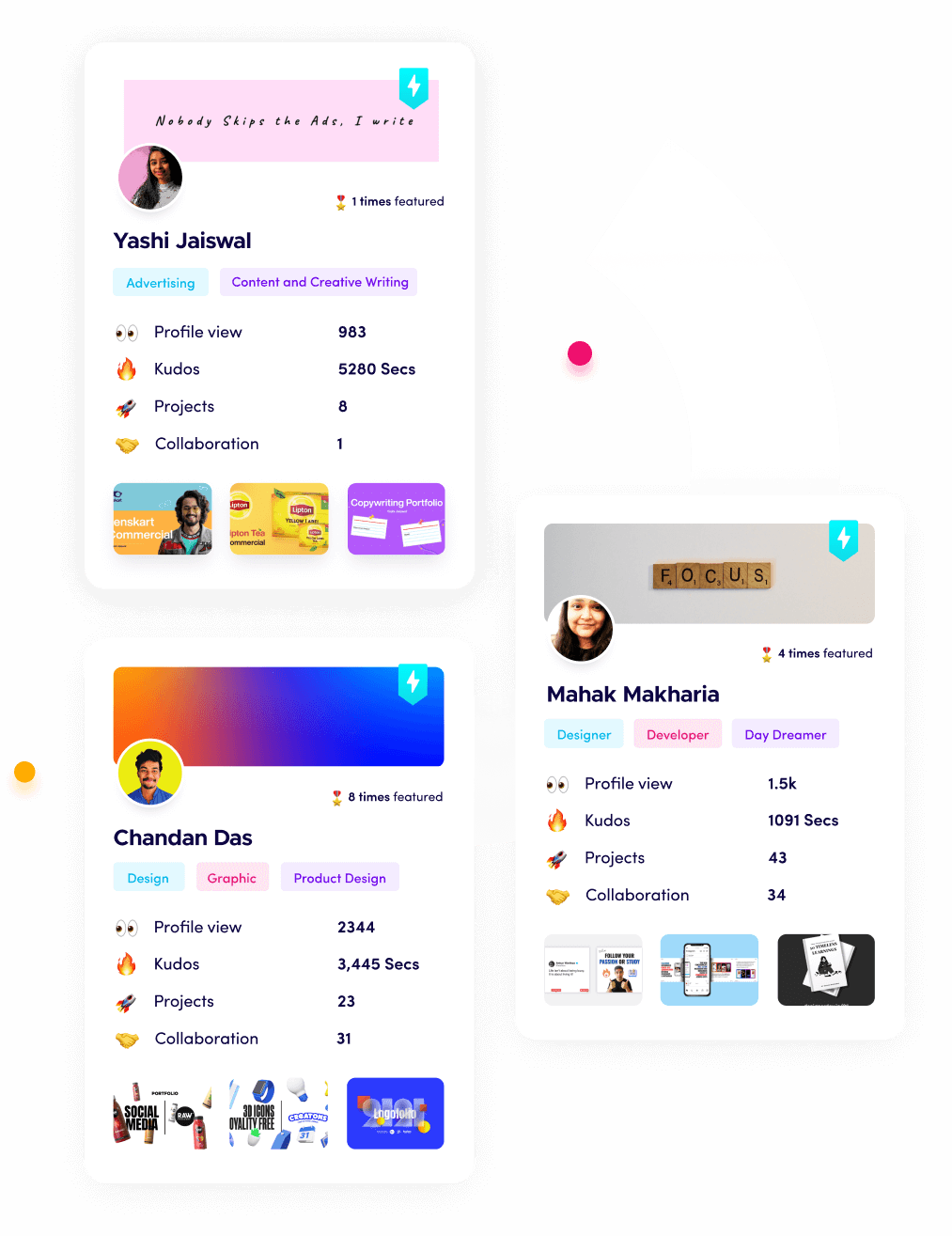
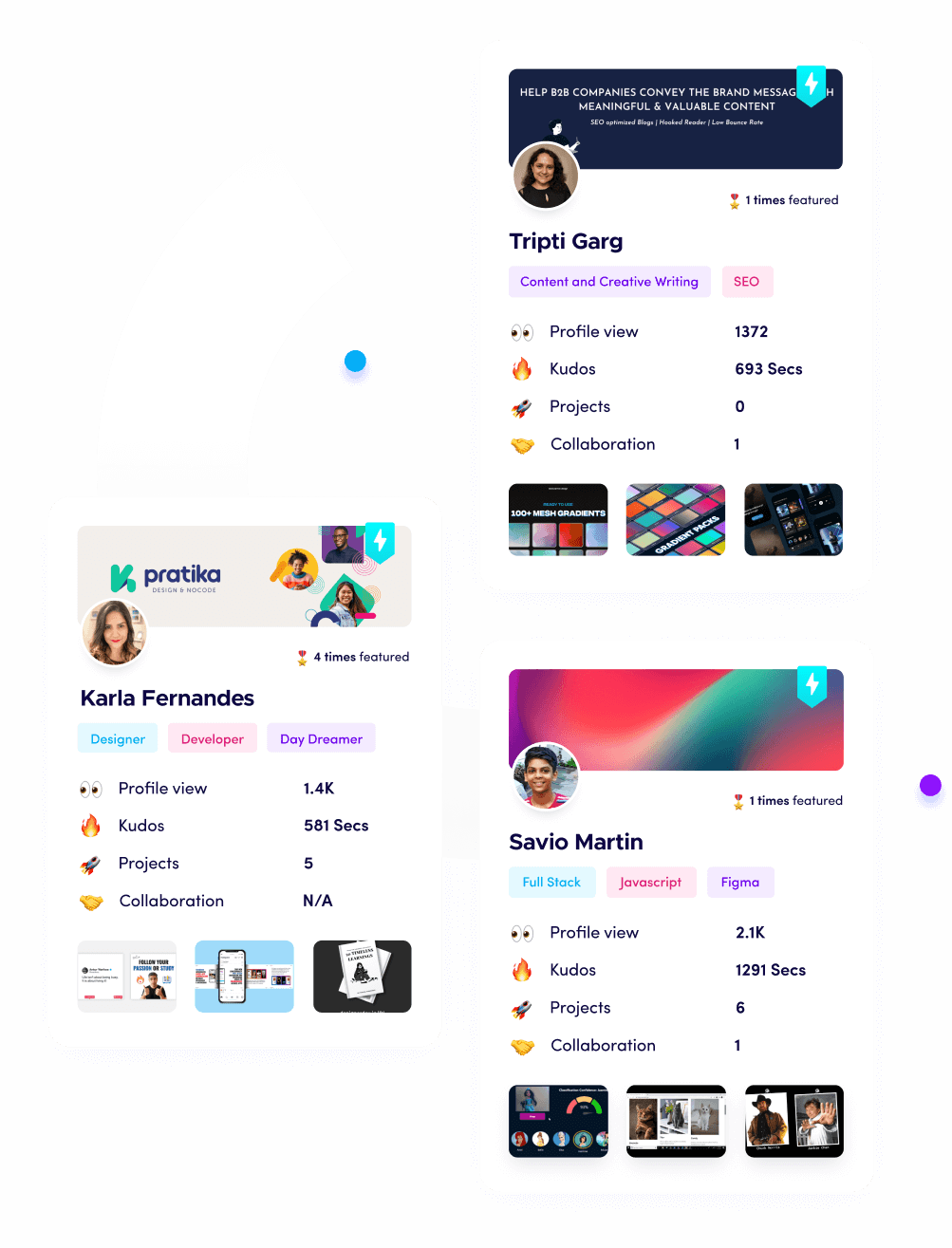
I’m Riten, the founder of Fueler - a skills-first portfolio platform that connects talented individuals with companies through assignments, portfolios, and projects, not just resumes/CVs. Think Dribbble/Behance for work samples + AngelList for hiring infrastructure.
1. Butterfly iQ3 Handheld Ultrasound
The Butterfly iQ3 represents the third generation of "ultrasound-on-a-chip" technology, which has effectively miniaturized a massive imaging machine into a device the size of an electric shaver. Unlike traditional ultrasound machines that require multiple expensive probes for different parts of the body, the iQ3 uses a single universal probe that can perform whole-body imaging, from deep abdominal scans to delicate vascular work. In 2026, this tool will have become a staple in US primary care and emergency clinics, as it allows doctors to instantly visualize internal organs during a standard physical exam. The device connects directly to a smartphone or tablet, utilizing AI-driven "Auto-Bladder" and "Auto-B-Line" tools to help clinicians who may not be full-time radiologists interpret images with high confidence.
- The iQ3 is powered by advanced "Biplane Imaging," which allows clinicians to see two planes of the body simultaneously in real-time, making it significantly easier to guide needles for biopsies or joint injections.
- Integrated AI software provides real-time guidance to the user, highlighting anatomical structures and even grading the quality of the image to ensure the most accurate diagnostic data is captured every time.
- The device is designed to be "drop-tested" and rugged, featuring a battery life that supports over two hours of continuous scanning, which is more than enough for a full day of typical clinical patient rotations.
- Data is automatically uploaded to the Butterfly Cloud, where it can be securely shared with specialists for a second opinion or integrated directly into the patient’s permanent Electronic Health Record (EHR).
- Recent 2026 firmware updates have introduced "Pulse-Wave Doppler" capabilities, allowing small clinics to perform basic cardiac and vascular flow assessments that were previously only possible in dedicated imaging suites.
Pricing: The handheld probe itself is priced at approximately $3,899 as a one-time hardware purchase, which is significantly more affordable than traditional $50,000 cart-based systems.
- Clinics typically pay an annual subscription for the software and cloud storage, which ranges from $420 per year for individual users to $3,500 per year for a five-user clinic license.
2. Eko CORE 500 Digital Stethoscope
The Eko CORE 500 has redefined the most iconic tool in medicine by combining high-fidelity digital acoustics with a 3-lead ECG and a full-color display on the chestpiece. This device is specifically designed to tackle the "silent" killers of heart disease by using AI to detect murmurs, AFib, and bradycardia in as little as 15 seconds during a routine checkup. In the busy environment of a 2026 clinic, its active noise cancellation technology is a game-changer, allowing doctors to hear clear heart and lung sounds even in a noisy hallway or a procedure room. By providing a visual waveform of the patient's heart rhythm directly on the stethoscope, it bridges the gap between a simple auscultation and a full diagnostic electrocardiogram.
- The device features "TrueSound" technology, which provides 40x amplification and 8-level volume control, making it an essential tool for clinicians with hearing loss or those working in high-decibel environments.
- A full-color LCD screen on the back of the chestpiece shows the patient's heart rate and ECG rhythm in real-time, allowing the doctor to spot arrhythmias without ever looking away from the patient.
- The Eko AI, cleared by the FDA, analyzes the captured sounds and rhythms to flag signs of heart failure or valvular heart disease with a level of sensitivity that far exceeds the human ear alone.
- It offers a "Wireless Listening" mode through Bluetooth, enabling clinicians to use high-quality noise-canceling headphones or hearing aids to listen to the patient’s heart while maintaining a comfortable distance.
- Every recording can be saved to a HIPAA-compliant app, allowing the doctor to track the progression of a heart murmur over several years or share the audio file directly with a cardiologist for a quick consult.
Pricing: The Eko CORE 500 is currently priced at $659 for the complete unit, which includes the digital chestpiece, the specialized earpieces, and access to the basic visualization app.
- For advanced AI-driven detection features and enterprise-level data management, clinics can subscribe to the "Eko+ Pro" software for approximately $50 to $75 per month per clinician.
3. Dexcom G7 Continuous Glucose Monitor (Clinic Edition)
The Dexcom G7 has moved beyond just a personal wearable for patients and is now a powerful "diagnostic" tool used within clinics to identify pre-diabetes and manage complex metabolic health. In 2026, many US clinics utilize the "Pro" version of the G7, where a patient wears the tiny, water-resistant sensor for ten days to provide the doctor with a complete "glucose map" of their life. This data is far more valuable than a single finger-stick test, as it shows how a patient's blood sugar reacts to specific foods, exercise, and stress. It allows for a "precision nutrition" approach where the doctor can offer evidence-based lifestyle advice that is unique to that specific patient’s biology.
- The G7 sensor is the size of three stacked quarters and features a "zero-warm-up" time, meaning it starts providing accurate glucose data almost the moment it is applied to the patient's arm in the clinic.
- The Dexcom Clarity software automatically generates a "Time in Range" report for the doctor, which is the 2026 gold standard for measuring how well a patient is managing their diabetes or metabolic health.
- It includes predictive alerts that can warn a patient of an impending "low" up to 20 minutes before it happens, providing a safety net that traditional testing methods simply cannot match.
- The device is fully integrated with most major insulin pumps and "smart" insulin pens, creating a closed-loop system that can automatically adjust medication doses based on the sensor's real-time data.
- For clinics, the "Professional" mode allows the sensor to be applied "blinded," meaning the patient doesn't see the data during the 10-day study, which provides a more accurate picture of their baseline lifestyle habits.
Pricing: For patients with insurance, the G7 is often available for a co-pay of $35 to $60 per month, while the "cash price" without insurance typically ranges from $170 to $200 per 30-day supply.
- Clinics purchasing "Pro" kits for diagnostic studies usually pay a bulk rate of approximately $150 to $300 per patient study, which often includes the sensor and the clinical data analysis report.
4. Nuance DAX Copilot (Ambient AI Scribe)
Nuance DAX Copilot is the leading "ambient" AI tool that has revolutionized clinical documentation across the United States. Rather than a physical piece of medical equipment, this is a sophisticated AI "listener" that runs on a clinician's smartphone or a dedicated exam room microphone. It securely captures the conversation between a doctor and patient and, within seconds of the visit ending, produces a perfectly formatted clinical note in the EHR. In 2026, this tool is the primary defense against physician burnout, as it eliminates the "pajama time" doctors used to spend typing notes late into the night, allowing them to focus entirely on the person sitting in front of them.
- The AI is trained to understand complex medical terminology and different accents, ensuring that it accurately captures everything from a detailed surgical history to a new medication plan discussed in the room.
- DAX Copilot doesn't just transcribe; it "reasons" through the conversation to create a structured "S.O.A.P." note, separating the patient’s symptoms (Subjective) from the doctor’s findings (Objective) and the final diagnosis (Plan).
- It features deep integration with major EHRs like Epic and Oracle Health, allowing the doctor to review, edit, and sign off on the AI-generated note directly within their existing digital workflow.
- The system is built with high-level encryption and does not "store" the audio recordings after the note is generated, ensuring that patient privacy is maintained at a level that meets the strictest HIPAA standards.
- In 2026, the software will have been updated to include "Order Suggestions," where the AI can prep prescriptions or lab orders based on what it heard the doctor say to the patient during the visit.
Pricing: DAX Copilot is typically sold through enterprise channels, with pricing sitting around $600 per clinician per month, though volume discounts are common for larger multi-specialty clinics.
- There is often a one-time implementation and "AI-training" fee for the clinic, which can range from $500 to $2,500 depending on the complexity of the EHR integration required.
5. Welch Allyn RetinaVue 350 (Teleretinal Camera)
The RetinaVue 350 is a handheld, non-mydriatic fundus camera that allows primary care clinics to perform professional-grade diabetic retinopathy screenings without needing to dilate the patient's eyes. In the US, where millions of diabetics miss their annual eye exams, this tool is a "life-saver" that brings specialized ophthalmology into the family practice. A medical assistant can take a high-resolution image of the patient’s retina in seconds, and the software uses AI to instantly check the image quality before transmitting it to a board-certified ophthalmologist for a remote reading. This "teleretinal" model ensures that patients with early signs of blindness are caught and referred to a specialist immediately.
- The camera is "non-mydriatic," meaning it can capture clear images through small pupils without the need for uncomfortable dilating drops, making it a much more pleasant experience for the patient.
- Integrated "proprietary image quality" software provides the operator with instant feedback on whether the photo is clear enough for a diagnosis, reducing the need for patient callbacks and repeat scans.
- The device is completely wireless and portable, allowing it to be easily moved between different exam rooms or even used in home-visit settings for elderly or homebound patients.
- Once the image is captured, it is transmitted via a secure network to the RetinaVue professional network, where a diagnostic report is typically returned to the clinic within 6 to 24 hours.
- This tool is highly favored by US insurance providers, as it significantly increases "quality scores" for clinics and helps prevent the massive long-term costs associated with untreated vision loss.
Pricing: The RetinaVue 350 hardware typically costs between $12,000 and $15,000, though many distributors offer "lease-to-own" programs for smaller independent practices.
- Clinics also pay a "per-report" fee for the ophthalmologist’s reading, which usually ranges from $15 to $30 per patient, and is often fully reimbursable through specialized Medicare and private insurance codes.
6. InBody 770 Body Composition Analyzer
The InBody 770 is a research-grade body composition analyzer that has become a "must-have" for US clinics focusing on longevity, obesity medicine, and sports rehabilitation. Unlike a standard scale that only measures total weight, the 770 uses "Bioelectrical Impedance Analysis" (BIA) to provide a deep dive into the patient’s internal health, measuring muscle mass, body fat percentage, and visceral fat levels. By 2026, this tool will be used to track the effectiveness of new weight-loss medications, ensuring that patients are losing fat rather than vital muscle mass. It provides a "Segmental Lean Analysis," showing the doctor exactly where a patient is gaining or losing muscle in each limb.
- The device uses six different frequencies to measure "Intracellular" and "Extracellular" water, which is a critical marker for identifying hidden inflammation, edema, and overall cellular health.
- It produces a comprehensive one-page "Result Sheet" that uses color-coded charts and graphs to make it easy for the patient to understand their progress and stay motivated with their treatment plan.
- The 770 features an "advanced" mode that tracks "Phase Angle," a measurement that correlates with cellular integrity and is increasingly used in 2026 as a general biomarker for biological age and vitality.
- The system is completely non-invasive and takes less than 60 seconds to complete a full scan, making it an easy add-on to a standard consultation or a specialized "wellness" visit.
- Data is stored in the cloud and can be synced with the clinic’s patient portal, allowing patients to track their body composition trends over time on their own smartphones.
Pricing: The InBody 770 is a premium clinical tool with a one-time hardware cost of approximately $18,000 to $22,000, making it a significant investment for a growing wellness practice.
- Ongoing costs are minimal, consisting mostly of the specialized "InBody tissues" and results paper, though some clinics opt for a $50 to $100 monthly subscription for advanced cloud data management.
7. BioFire FilmArray (Point-of-Care PCR)
The BioFire FilmArray has brought "molecular-level" laboratory testing directly into the clinic, allowing doctors to diagnose infectious diseases with 99% accuracy in about an hour. Instead of sending a swab to a distant lab and waiting three days for results, a clinician can use the FilmArray to test for dozens of viruses and bacteria, including the flu, COVID-19, and strepall at once. In the 2026 "post-pandemic" era, this tool is essential for clinics that want to provide immediate answers and ensure that antibiotics are only prescribed when they are truly necessary. This "syndromic" approach to testing saves time, reduces patient anxiety, and helps fight the global crisis of antibiotic resistance.
- The system uses "nested PCR" technology, which is considered the gold standard in molecular biology, providing results that are far more accurate than the "rapid" antigen tests found in drugstores.
- BioFire offers various "panels," such as the Respiratory Panel or the Gastrointestinal Panel, which can test for up to 22 different pathogens from a single patient sample simultaneously.
- The software is designed for "ease of use," requiring only two minutes of "hands-on" time from a medical assistant to prepare the sample and start the automated run in the machine.
- In 2026, the FilmArray is frequently used in "urgent care" settings to quickly differentiate between a simple cold and a more serious bacterial infection that requires immediate hospital admission.
- The device is fully "closed-system," meaning there is zero risk of sample contamination, which is a common problem with traditional manual PCR testing in smaller clinical labs.
Pricing: The BioFire "Torch" system (the hardware unit) generally starts at around $25,000 to $45,000, depending on the number of modules a clinic needs to run tests simultaneously.
- The individual "test pouches" (the single-use chemical kits) are the ongoing cost, typically ranging from $120 to $180 per test, which are usually covered by insurance under specific molecular diagnostic codes.
8. HeartFlow FFRCT Analysis (AI Cardiac Imaging)
HeartFlow is a non-invasive AI technology that has changed how US cardiologists diagnose coronary artery disease without needing to perform a dangerous and expensive heart catheterization. While the "hardware" is a standard CT scanner, the HeartFlow software uses "computational fluid dynamics" and AI to create a personalized 3D model of a patient's heart. This model allows doctors to see exactly how blood is flowing through the arteries and identify which blockages are actually restricting flow and which ones are harmless. By 2026, this "digital stress test" has become the preferred first step for patients with chest pain, as it provides more information than a traditional treadmill test with zero physical risk.
- The AI model provides a numerical value (FFRCT) for every branch of the coronary arteries, showing the doctor exactly where the pressure drops are occurring and where a stent might be needed.
- This technology has been shown to reduce "unnecessary" invasive heart procedures by over 60%, as it can accurately identify patients who can be treated with medication alone.
- HeartFlow’s 2026 update includes "Plaque Analysis," which can distinguish between "hard" calcified plaque and "soft" vulnerable plaque that is more likely to cause a sudden heart attack.
- The system is a cloud-based service; a clinic simply uploads the patient's CT scan to HeartFlow’s secure servers, and the 3D model is returned to the doctor’s computer within a few hours.
- It is backed by the American College of Cardiology (ACC) and is now a "standard of care" recommendation for the evaluation of stable chest pain in the United States.
Pricing: Clinics and hospitals do not typically buy the software; instead, they pay a "per-patient" analysis fee, which in 2026 is approximately $1,000 to $1,500 per case.
- Most of this cost is reimbursed by Medicare and private insurance providers, often paying the facility around $850 to $1,100 per study to cover the technical and professional interpretation.
9. Omron HeartGuide (Clinical-Grade BP Smartwatch)
The Omron HeartGuide is the first wearable blood pressure monitor that has been clinically validated to be as accurate as the "cuff" in a doctor’s office. Unlike other smartwatches that "estimate" blood pressure using light sensors, the HeartGuide features a miniature inflatable cuff inside the wristband that physically compresses the artery. In 2026, US clinics will prescribe these watches to patients with "resistant hypertension" or those who suffer from "white-coat syndrome" (high blood pressure only when at the doctor). It provides the clinician with a 24/7 view of the patient's blood pressure throughout the day and night, ensuring that medications are actually working in the real world.
- The watch uses "oscillometric" measurement technology, which is the same method used by professional-grade medical monitors, making it the only "medical-grade" BP wearable on the US market.
- It automatically tracks blood pressure, activity, and sleep, allowing the doctor to see how a patient’s lifestyle choices like a high-sodium meal or a stressful workday impact their heart health.
- The "Omron Connect" app allows patients to instantly share their 7-day or 30-day average blood pressure reports with their doctor via a secure PDF, eliminating the need for manual "BP logs."
- In 2026, the device features "nighttime monitoring," which is critical for identifying "non-dippers" patients whose blood pressure stays high at night, which is a major risk factor for stroke.
- The battery lasts for approximately two to three days on a single charge and is designed to look like a high-end luxury watch, which significantly increases patient "compliance" compared to traditional bulky monitors.
Pricing: The Omron HeartGuide is available for clinics to purchase or for patients to buy directly for approximately $499 to $550 as a one-time hardware cost.
- Some clinics offer these through a "Remote Patient Monitoring" (RPM) program, where the cost of the watch and the monitoring service is covered by insurance for about $120 per month.
10. Nonin Onyx Vantage 9590 Pulse Oximeter
While pulse oximeters became common during the pandemic, the Nonin Onyx Vantage 9590 remains the "clinical standard" for US doctors who need absolute accuracy in the most challenging conditions. Unlike cheap consumer sensors, the 9590 is designed to work on patients with dark skin tones, poor circulation, or high levels of motion in situations where other sensors often fail or provide false readings. In 2026, this device is the "go-to" for US pulmonary and pediatric clinics where a wrong oxygen reading can lead to an unnecessary emergency room visit. Its "PureSAT" technology filters out "noise" to provide a pulse-by-pulse reading that is trusted for critical medical decisions.
- The 9590 is built to be "indestructible," surviving hundreds of drops and thousands of uses in a busy clinic environment, which is why it often comes with a 4-year "bumper-to-bumper" warranty.
- It is "lead-free" and "latex-free," making it safe for all patient populations, including those with severe allergies or sensitivities.
- The device features a unique "pulse quality" indicator green, yellow, or red light that tells the clinician immediately if the sensor has a good enough signal to provide a reliable reading.
- In 2026, the sensor was updated with "Bluetooth Low Energy," allowing it to transmit oxygen data directly to a tablet for "spot-checking" patients in a triage line without needing any wires.
- It is one of the few handheld sensors that is cleared by the FDA for "all-day" monitoring, meaning it can be used for "six-minute walk tests" to assess a patient’s lung function under stress.
Pricing: The Nonin Onyx Vantage 9590 is priced at approximately $180 to $225 per unit, making it more expensive than consumer models but significantly more durable for clinical use.
- There are no ongoing subscription fees for this device, making it a "buy-it-and-forget-it" tool with a total cost of ownership that is very low over its 5-to-7-year lifespan.
11. Proteus Discover (Digital Medicine System)
Proteus Discover is an "Ingestible Sensor" technology that has entered the clinical mainstream in 2026 to solve the problem of "medication non-adherence." This system involves a tiny, sand-grain-sized sensor that is added to a patient’s pill. When the patient swallows the medication, the sensor is activated by stomach acid and sends a signal to a small patch worn on the patient's skin. This patch then logs the exact time the medication was taken and transmits that data to the clinic. This is particularly vital for patients taking high-stakes medications for organ transplants, severe mental health conditions, or infectious diseases like tuberculosis.
- The sensor is made of minerals found in food and is naturally digested and passed through the body, making it a completely safe and non-invasive way to track drug "compliance."
- The skin patch also tracks the patient's heart rate, steps, and sleep patterns, giving the doctor a 360-degree view of how the patient is "responding" to the medication in real-time.
- If a patient misses a critical dose, the system can send an automated text reminder to the patient or an alert to their family caregiver or clinical pharmacist.
- In 2026, US clinical trials showed that patients using "Digital Medicines" have a 40% higher chance of reaching their health goals compared to those using traditional pill bottles.
- This technology is increasingly used in "Value-Based" contracts, where the pharmaceutical company only gets paid if the patient actually takes the medicine as prescribed and sees a clinical benefit.
Pricing: The "Discover" system is typically sold to clinics and health systems as a "service," with costs ranging from $150 to $250 per patient per month.
- Many insurance providers are beginning to cover this as part of a "Chronic Care Management" (CCM) program, recognizing the massive savings from preventing hospitalizations caused by missed medications.
12. Welch Allyn Spot Vision Screener
The Spot Vision Screener is a handheld, "camera-like" device that can perform a comprehensive eye exam on children as young as six months old in about three seconds. In 2026, this tool has become the standard for US pediatric clinics, as it can detect major vision problems like "lazy eye" (amblyopia), nearsightedness, and farsightedness from a distance of three feet. Traditional eye charts are useless for toddlers who can't read or speak, but the "Spot" uses lights and sounds to capture the child's attention and automatically scans their eyes to provide a "pass/fail" result instantly. This ensures that every child is screened for vision issues long before they start school.
- The device uses "automated binocular screening," meaning it tests both eyes at the same time and can detect issues like "anisometropia" (when one eye is significantly weaker than the other).
- It features a simple "Stop-and-Go" touchscreen interface that is so easy to use that a medical assistant or a volunteer can perform the screenings with minimal training.
- The software automatically generates a "Parent-Friendly" report that can be printed or emailed, explaining the results in simple language and advising if a follow-up with a specialist is needed.
- In 2026, the device is fully integrated with school health databases, allowing for "mass-screenings" where hundreds of children can be tested in a single afternoon with all data automatically recorded.
- It is designed to work in "challenging" environments, such as low-light rooms or with patients who have limited mobility, making it a highly versatile tool for any clinical setting.
Pricing: The Welch Allyn Spot Vision Screener is a specialized pediatric tool with a hardware cost of approximately $8,500 to $10,500.
- There are no "per-test" fees, and many clinics recover the initial cost within the first year by billing insurance for "Instrument-Based Vision Screening" (CPT code 99177), which typically pays $25 to $40 per child.
Final Thoughts
The medical tools of 2026 are defined by their ability to "listen" and "see" more than ever before. For a modern US clinic, the transition to these digital and AI-powered devices is no longer a luxury but a necessity for staying competitive in a fast-moving healthcare market. By moving expensive diagnostics out of the hospital and into the neighborhood clinic, these tools are making healthcare more convenient for patients and more rewarding for clinicians. While the initial investment in devices like the Butterfly ultrasound or the BioFire PCR system can be significant, the long-term benefits of faster diagnoses, higher reimbursement rates, and improved patient trust make them the foundation of modern medical practice.
Frequently Asked Questions
Are these handheld medical tools as accurate as traditional hospital machines?
In 2026, yes. Most of these handheld devices, such as the Butterfly iQ3 and the Eko CORE 500, have undergone rigorous clinical trials and have been cleared by the FDA as "clinically equivalent" to their larger predecessors. While they may not have all the "bells and whistles" of a $500,000 hospital system, they provide more than enough diagnostic power for 95% of clinical scenarios.
Can a small clinic really afford these high-tech tools?
Many of these tools are designed with "Return on Investment" (ROI) in mind. For example, while the BioFire FilmArray is expensive, it allows a clinic to bill for complex lab testing that they previously had to "give away" to a third-party lab. Additionally, many vendors now offer "subscription-based" hardware models that allow a clinic to get the latest tools for a manageable monthly fee rather than a large upfront payment.
Do these tools require a lot of technical training for clinic staff?
The "magic" of 2026 medical technology is that it is designed to be "user-friendly." Most of these devices, like the Spot Vision Screener or Nuance DAX, use AI to handle the "complex" parts of the job, such as interpreting an image or formatting a note. This means that a medical assistant or a nurse can perform much of the "data gathering" with just a few hours of training, allowing the doctor to focus purely on the final diagnosis.
How is patient privacy protected on these connected devices?
Every device listed above is built to "Enterprise-Grade" security standards. They use end-to-end encryption, multi-factor authentication (MFA), and are fully HIPAA-compliant. In most cases, patient data is "anonymized" before being sent to the cloud for AI analysis, and the actual audio or images are never stored on the individual device itself, making them much more secure than older "analog" paper records.
Is insurance reimbursement available for these new technologies?
Yes, the US healthcare system has evolved to support these tools. There are specific "CPT codes" (billing codes) for things like "Remote Patient Monitoring," "Point-of-Care Ultrasound," and "Digital Vision Screening." In many cases, the insurance reimbursement is high enough that the device pays for itself within the first 100 to 200 uses, making it a financially sound move for any growing clinic.
What is Fueler Portfolio?
Fueler is a career portfolio platform that helps companies find the best talent for their organization based on their proof of work. You can create your portfolio on Fueler. Thousands of freelancers around the world use Fueler to create their professional-looking portfolios and become financially independent. Discover inspiration for your portfolio
Sign up for free on Fueler or get in touch to learn more.