Top 15 Health Technology Innovations in the United States in 2026

Riten Debnath
16 Jan, 2026

Imagine a world where your doctor can predict a health issue before you even feel a symptom, or where a surgeon performs a life-saving operation from thousands of miles away using a high-precision robotic arm. This isn't science fiction anymore, as the United States is currently leading a massive shift in how we treat, monitor, and manage human health through groundbreaking technology. From artificial intelligence that reads X-rays better than humans to wearable devices that track every heartbeat, these innovations are making healthcare faster, cheaper, and much more personal for everyone.
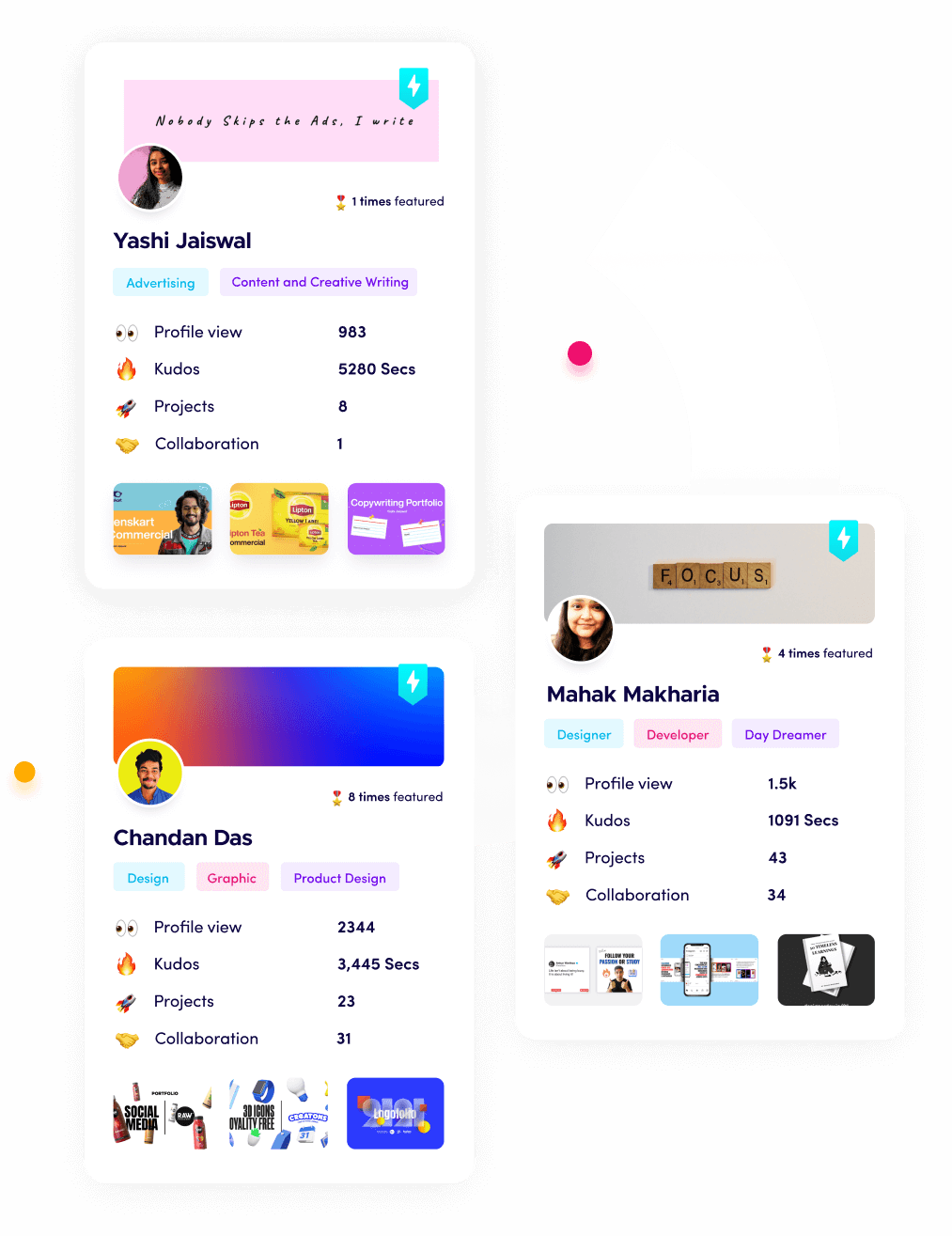
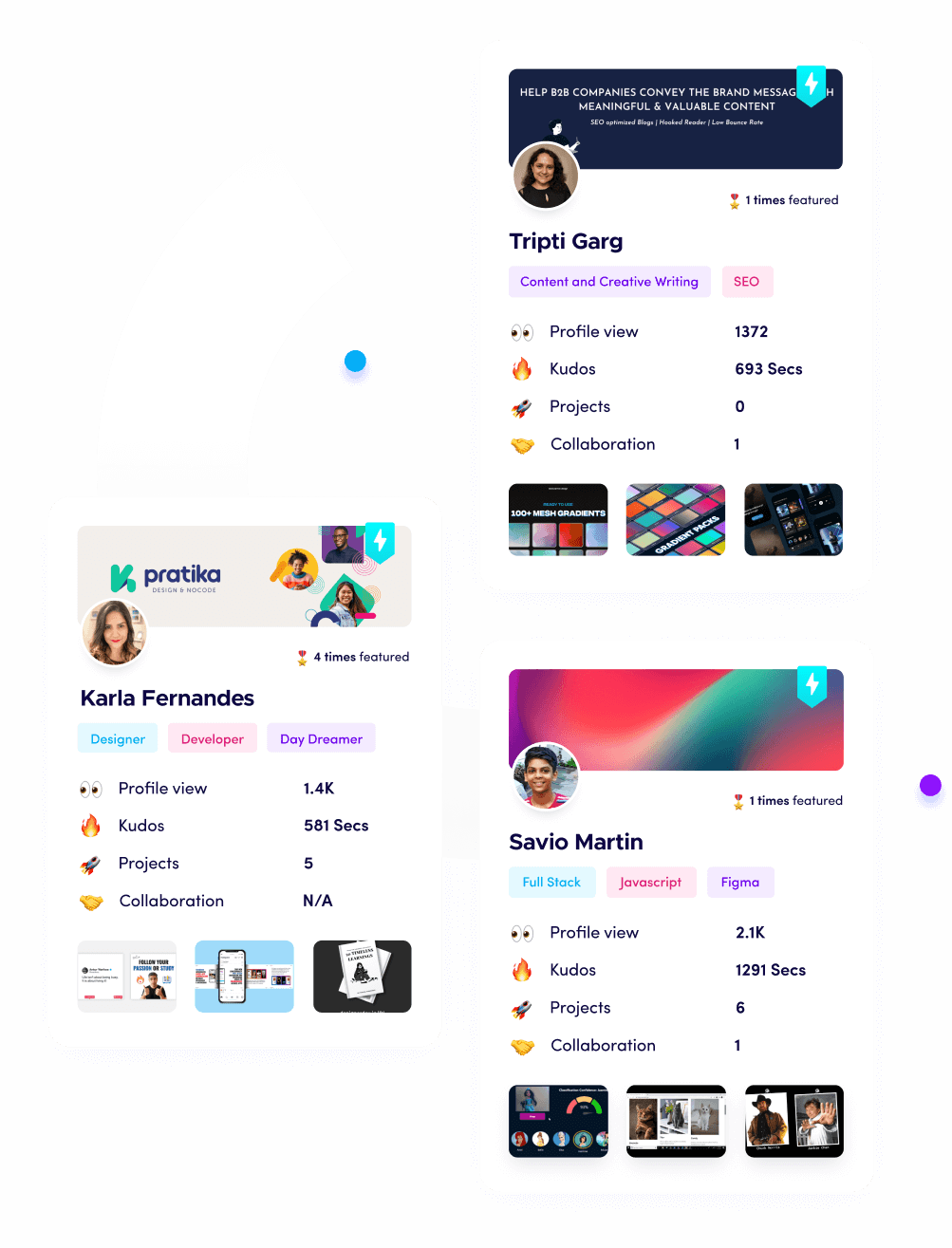
I’m Riten, the founder of Fueler - a skills-first portfolio platform that connects talented individuals with companies through assignments, portfolios, and projects, not just resumes/CVs. Think Dribbble/Behance for work samples + AngelList for hiring infrastructure
1. Ambient Clinical Intelligence (AI Medical Scribes)
Ambient Clinical Intelligence is a revolutionary shift in the doctor-patient relationship, designed to end the "keyboard between the doctor and patient" problem. These AI-powered tools use high-fidelity microphones to listen to the conversation in the exam room and automatically convert that natural dialogue into a structured medical note within the electronic health record. This technology is a response to the massive burnout crisis in the US, where physicians spend nearly two hours on paperwork for every one hour spent with a patient. By 2026, this technology has become the standard for modern clinics, allowing doctors to maintain eye contact and focus entirely on the human being in front of them while the software handles the complex coding.
- The software uses advanced natural language processing to distinguish between small talk about the weather and critical medical information such as symptoms or new medication dosages.
- These systems are built with multi-party recognition technology, meaning they can accurately identify and attribute statements to the doctor, the patient, and even a family member present in the room.
- The tool automatically maps the conversation to specific medical codes, which ensures that insurance billing is accurate and that the clinic remains compliant with the latest healthcare regulations.
- Many platforms now offer real-time clinical decision support, subtly flagging potential drug interactions or missing screening questions directly on the doctor's tablet during the patient visit.
- Security is handled through end-to-end encryption and HIPAA-compliant data silos, ensuring that these private conversations are never used for advertising or shared outside of the medical team.
Pricing: Individual licenses for tools like Abridge or Nuance DAX typically range from $250 to $600 per month per physician.
- For large health systems, enterprise-wide implementation can cost between $50,000 and $250,000, depending on the number of active users and integration depth.
- Many vendors offer a tiered model where basic transcription is cheaper, but the advanced AI-coding and analytics features require a premium subscription.
Why it matters: This innovation is critical because it addresses the mental health and retention of our healthcare workforce. By removing the administrative burden, we allow doctors to return to the "art of medicine," which leads to more accurate diagnoses and a significantly better experience for the patient.
2. Generative AI for Accelerated Drug Discovery
Traditional drug development has historically been a slow and incredibly expensive process, often taking over a decade and billions of dollars to bring a single medicine to market. Generative AI is changing this by using massive datasets to simulate how new drug molecules will interact with human cells before a single physical experiment is even conducted in a lab. This allows pharmaceutical companies to identify promising candidates in a fraction of the time, potentially bringing life-saving treatments for rare diseases to patients years earlier than before. By 2026, the US biotech sector will have integrated these "digital labs" into the very core of its research and development strategies.
- The AI can analyze millions of protein structures and chemical compounds simultaneously to predict which ones will successfully bind to a disease target without causing harmful side effects.
- Researchers use generative models to design entirely new molecules that do not exist in nature, specifically engineered to attack complex cancers or neurodegenerative conditions like Alzheimer's.
- This technology significantly reduces the "failure rate" of clinical trials by identifying potential toxicity issues early in the simulation phase, saving companies millions of dollars in wasted research.
- Multi-modal AI systems can now combine genetic data with chemical modeling to create "personalized" drug candidates that are optimized for specific patient populations or genetic markers.
- The software allows for the creation of "synthetic control arms" in clinical trials, which can reduce the number of human participants needed and speed up the FDA approval process.
Pricing: Access to specialized drug discovery platforms like Insilico Medicine or Recursion often involves multi-million dollar partnership agreements rather than simple monthly fees.
- For smaller research labs, cloud-based AI tools from providers like AWS HealthLake can start at $0.50 per hour for basic compute resources plus data storage fees.
- Enterprise SaaS licenses for AI-driven laboratory management systems can range from $5,000 to $20,000 per month for mid-sized pharmaceutical teams.
Why it matters: In the United States, the high cost of prescription drugs is a major political and social issue. By making the discovery process more efficient and less prone to failure, this technology creates a pathway for more affordable and diverse treatments for the most challenging medical conditions.
3. Remote Patient Monitoring (RPM) with IoMT
The Internet of Medical Things (IoMT) has moved healthcare out of the hospital and into the living room, allowing for continuous monitoring of chronic conditions. Remote Patient Monitoring uses a network of connected devices, such as blood pressure cuffs, glucose monitors, and smart scales, that transmit data in real-time to a patient's care team. This is particularly vital in the US, where chronic diseases like diabetes and heart failure account for the vast majority of healthcare spending. Instead of waiting for a crisis, doctors can now intervene the moment a patient's data starts to trend in a dangerous direction.
- These devices are often cellular-enabled, meaning they work right out of the box without the patient needing to have a smartphone or complex home Wi-Fi setup.
- The software platforms use "red-flag" algorithms to alert nurses or doctors only when a reading is outside of a safe range, preventing clinicians from being overwhelmed by normal data.
- RPM platforms integrate directly with major Electronic Health Records, ensuring that the data collected at home becomes a permanent part of the patient's official medical history.
- Many systems include "gamification" features that encourage patients to take their readings daily, often providing rewards or positive feedback to help improve long-term adherence to treatment plans.
- The technology supports "Hospital-at-Home" programs, allowing patients to recover from surgeries or mild illnesses in their own beds while still being under 24/7 digital surveillance.
Pricing: The cost for an RPM software platform typically ranges from $20 to $50 per patient per month.
- Hardware costs for a basic "kit" (tablet plus two or three sensors) can range from $200 to $600 per patient as a one-time purchase or lease.
- Many providers in the US recoup these costs through Medicare reimbursement codes, which can pay the clinic between $100 and $150 per month per participating patient.
Why it matters: This innovation is the key to managing an aging population. By keeping patients stable at home and preventing expensive emergency room visits, RPM is one of the few technologies that can both improve health outcomes and lower the total cost of care.
4. Robotic-Assisted Surgery (RAS) with Haptic Feedback
Robotic surgery has evolved from a niche technology to a standard of care for many complex procedures in the United States. Modern systems like the da Vinci 5 allow surgeons to operate through tiny incisions with a level of precision and stability that exceeds the human hand. These robots do not replace the surgeon; rather, they act as a high-tech interface that provides 3D high-definition views and "wristed" instruments that can rotate in ways human fingers cannot. The latest 2026 models have introduced advanced haptic feedback, allowing the surgeon to actually "feel" the resistance of the tissue they are working on through the robotic console.
- The system's feature advanced "tremor filtration" software that removes even the slightest hand shake, ensuring that every movement of the surgical tool is perfectly smooth and intentional.
- 3D visualization systems provide 10x magnification, allowing surgeons to see delicate nerves and blood vessels that would be nearly invisible during a traditional open surgery.
- Integrated AI overlays can highlight anatomical structures in real-time, helping the surgeon navigate around critical areas like the ureters or major arteries during a procedure.
- The latest robotic platforms are modular, meaning they can be easily moved between different operating rooms and reconfigured for different specialties like urology, gynecology, or thoracic surgery.
- Data from every robotic surgery is recorded and analyzed by AI, providing surgeons with a "scorecard" that helps them refine their technique and improve patient outcomes over time.
Pricing: A full surgical robotic system typically costs between $1.5 million and $2.5 million as an upfront purchase.
- Hospitals also pay an annual service contract, which usually ranges from $150,000 to $200,000 per year.
- Disposable instruments used for each specific surgery can add an additional $1,000 to $3,500 to the cost of every procedure performed.
Why it matters: Robotic surgery matters because it significantly reduces recovery times and the risk of infection. For the patient, this means shorter hospital stays and a faster return to work and family, which is a major economic and personal benefit in the American healthcare system.
5. Digital Twins of the Human Body
Digital twin technology creates a virtual, data-driven replica of a patient’s specific organs or their entire biological system. By combining medical imaging, genetic data, and real-time sensor readings, doctors can "test" a surgery or a specific medication on the digital twin before ever touching the actual patient. This is moving healthcare toward true "precision medicine," where treatments are no longer based on population averages but on the unique physics and biology of the individual. In 2026, this technology is being used extensively in cardiology to model heart blood flow and in oncology to predict how a specific tumor will respond to chemotherapy.
- The digital twin is constantly updated with new data, meaning it evolves as the patient ages or as their health condition changes over the course of several years.
- Surgeons use these 3D models to perform "practice runs" of complex operations, allowing them to identify potential complications and map out the safest route before the patient enters the room.
- In pharmaceutical research, digital twins of the heart or liver are used to screen new drugs for potential toxicity, reducing the need for animal testing and human clinical trials.
- The models can simulate "what-if" scenarios, such as how a patient's risk of a stroke might change if they started a new exercise routine or changed their diet over the next six months.
- Computational fluid dynamics are used within the twin to predict how blood will flow through a new stent or heart valve, helping doctors choose the perfect size and placement for the device.
Pricing: Specialized software for single-organ digital twins (like the heart) can cost clinics between $15,000 and $40,000 per year in licensing fees.
- For large research institutions, enterprise-level modeling platforms can reach $250,000 or more annually.
- Some consumer-focused digital twin services for "longevity" and health optimization are now available for $2,500 to $5,000 per scan and analysis.
Why it matters: This technology eliminates the "trial and error" approach to medicine. In the US, where medical errors and ineffective treatments are major contributors to healthcare costs, digital twins provide a safety net that ensures the right treatment is delivered the first time.
6. CRISPR-Cas9 and Next-Gen Gene Editing
CRISPR technology has moved from the laboratory to the clinic, offering the potential to actually "cure" genetic diseases rather than just managing their symptoms. This technology acts like a pair of molecular scissors, allowing scientists to go into a patient's DNA and cut out or repair a faulty gene that is causing a disease. In the United States, we have seen the first FDA-approved CRISPR treatments for conditions like Sickle Cell Anemia, marking a historic turning point in human medicine. By 2026, the focus has shifted toward using AI to make gene editing even safer by ensuring the "scissors" only cut at exactly the right location.
- The technology can be used to "turn off" genes that cause high cholesterol or to "program" a patient's own immune cells to seek out and destroy specific types of cancer cells.
- Next-generation "base editing" allows for even finer control, changing a single "letter" of the genetic code without needing to break the DNA strand entirely.
- Clinical applications are expanding into common conditions like cardiovascular disease, where a one-time genetic "tune-up" could potentially provide lifelong protection against heart attacks.
- Delivery systems for CRISPR are becoming more sophisticated, using specialized nanoparticles to carry the gene-editing tools directly to the specific organ that needs treatment, such as the liver or the eye.
- The software used to design these genetic edits now incorporates AI to predict and prevent "off-target" effects, which are unintended changes to other parts of the patient's DNA.
Pricing: CRISPR treatments are currently among the most expensive medical procedures in the world, often costing between $2 million and $3 million for a one-time cure.
- The software and laboratory tools for researchers to design edits typically cost $10,000 to $30,000 per year for a standard lab license.
- Insurance companies in the US are currently developing "annuity-based" payment models to help spread the high cost of these one-time cures over several years.
Why it matters: While the cost is high, CRISPR is a game-changer because it represents the end of lifelong chronic illness for many patients. A one-time multi-million dollar treatment can actually be cheaper for the healthcare system than decades of hospitalizations, medications, and lost productivity.
7. Extended Reality (XR) for Medical Training and Therapy
Extended Reality, which includes Virtual Reality (VR) and Augmented Reality (AR), is transforming both how doctors learn and how patients recover. For medical students, VR provides a risk-free environment to practice rare or dangerous procedures as many times as they need to achieve mastery. On the patient side, VR is being used as a powerful "digital therapeutic" to treat chronic pain, anxiety, and PTSD by immersing the patient in calming or rehabilitative environments. By 2026, many US hospitals have established "XR Labs" as a standard part of their clinical and educational infrastructure.
- AR headsets are now used during live surgeries to overlay a patient's MRI or CT scans directly onto their body, giving the surgeon "X-ray vision" to see exactly where a tumor is located.
- VR-based rehabilitation programs for stroke patients use motion-tracked games to help people regain coordination and strength in a way that is much more engaging than traditional physical therapy.
- Medical schools are using XR to provide "virtual anatomy" classes, where students can walk through a giant, 3D model of the human heart and see how valves function in real-time.
- For pediatric patients, VR is used as a highly effective distraction tool during painful procedures like dressing changes for burns or vaccinations, significantly reducing the need for sedative medications.
- Remote collaboration platforms allow a specialist in New York to "scrub in" to a surgery in rural Montana via an AR headset, providing real-time guidance and advice to the local surgical team.
Pricing: Professional medical XR headsets like the HoloLens 2 or specialized VR systems cost between $3,500 and $5,000 per unit.
- Software subscriptions for medical training or patient therapy modules typically range from $500 to $2,000 per month per facility.
- Consumer-grade VR therapy apps for home use are now being prescribed by doctors, with monthly costs ranging from $30 to $100 often covered by insurance.
Why it matters: XR technology solves the problem of "access to expertise." It allows for high-level training and specialized care to be delivered anywhere, which is vital for rural hospitals in the US that may not have full-time access to world-class specialists or expensive training facilities.
8. Quantum Computing for Precision Pharma
Quantum computing is the newest frontier in healthcare technology, moving beyond the limits of traditional "binary" computers. While a standard computer sees the world in ones and zeros, a quantum computer can model the incredibly complex and chaotic world of subatomic particles. This makes them perfect for "folding" proteins and simulating how complex drugs will behave at a molecular level with perfect accuracy. In 2026, the first "quantum-classical" workflows have moved from theoretical labs into actual pharmaceutical pilots in the US, promising to solve medical puzzles that would take a normal computer thousands of years to figure out.
- Quantum algorithms can simulate the entire chemical reaction of a drug within a human cell, allowing for the discovery of medicines that are 100% effective with zero side effects.
- These computers are used to optimize hospital logistics, such as the massive task of scheduling thousands of staff members and matching them with patient flow in real-time across a national hospital network.
- In genomics, quantum computing can analyze the entire human genome for thousands of patients simultaneously to identify the hidden patterns that lead to rare diseases.
- The technology is being used to develop "ultra-secure" healthcare networks that are immune to traditional hacking and ransomware, protecting sensitive patient data at the highest level.
- Quantum sensors are also being developed that can detect tiny changes in a patient's magnetic field, allowing for the diagnosis of heart or brain issues much earlier than current MRI technology.
Pricing: Most healthcare companies access quantum power through "Quantum as a Service" (QaaS) from providers like IBM or Google, with costs starting at $1,000 per hour of compute time.
- Strategic partnerships for quantum drug discovery can involve upfront investments of $5 million to $15 million for a multi-year project.
- As the technology matures, dedicated quantum-inspired software for smaller labs is beginning to enter the market at around $5,000 per month.
Why it matters: Quantum computing is the ultimate "accelerator." It doesn't just improve on current technology; it allows us to ask and answer entirely new questions about human health, paving the way for the next century of medical breakthroughs that were previously thought to be impossible.
9. 3D Bioprinting of Human Tissue
3D Bioprinting has advanced from printing plastic models to printing living, functional human tissue. This technology uses "bio-inks" made of living cells to build structures like skin for burn victims, cartilage for knee repairs, and even small "organoids" for drug testing. The ultimate goal, which is becoming more realistic by 2026, is to print entire, transplantable organs like kidneys or livers using a patient's own cells, which would completely eliminate the organ donor shortage and the risk of transplant rejection. Currently, US medical centers are already using printed tissue to help heal complex wounds and reconstructive surgeries.
- The bioprinter uses a specialized nozzle to layer living cells with a supportive gel, creating a 3D structure that can eventually grow its own blood vessels and integrate with the patient's body.
- Researchers are printing "tumors-on-a-chip," which are 3D replicas of a specific patient's cancer that can be used to test dozens of different drugs to see which one works best before treating the patient.
- This technology is being used in dentistry to print custom, biocompatible jawbone inserts and dental implants that fit the patient's anatomy perfectly and promote faster healing.
- For drug companies, bioprinted liver and kidney tissues are becoming the standard for safety testing, as they provide a much more accurate reaction than traditional cell cultures or animal models.
- Advanced bioprinters can now print skin directly onto a patient's wound in the operating room, using a "skin gun" approach that can heal severe burns much faster than traditional skin grafts.
Pricing: High-end research-grade bioprinters cost between $100,000 and $400,000 as a one-time purchase for a laboratory.
- The "bio-ink" and specialized cartridges needed for a single tissue printing session can cost between $500 and $2,000 depending on the cell types involved.
- Clinical procedures involving 3D printed tissue are still largely in the trial phase, but costs are estimated to be $20,000 to $50,000 for specialized reconstructive surgeries.
Why it matters: This innovation addresses one of the most tragic problems in US healthcare, the organ shortage. By eventually being able to print an organ on demand using a patient's own cells, we can save thousands of lives every year and remove the need for patients to take immunosuppressant drugs for the rest of their lives.
10. AI-Powered Medical Imaging and Diagnostics
Medical imaging, such as MRIs, CT scans, and X-rays, has become so complex that human radiologists are often overwhelmed by the sheer volume of data. AI-powered diagnostic tools act as a "second pair of eyes" that never gets tired and can spot patterns that are invisible to the human eye. These systems can analyze thousands of images in seconds, flagging urgent cases like strokes or internal bleeding so that they can be treated immediately. In 2026, the US FDA cleared hundreds of these AI algorithms, making them a standard part of the diagnostic workflow in almost every major American hospital.
- AI algorithms can detect early-stage lung cancer or breast cancer much earlier than traditional methods, often spotting tiny abnormalities years before they would become symptomatic.
- The software can "denoise" low-quality images, allowing for faster and lower-radiation scans that are still clear enough for a perfect diagnosis, which is much safer for pediatric and elderly patients.
- In the emergency room, AI automatically prioritizes the worklist for radiologists, ensuring that life-threatening conditions like a pulmonary embolism are read within minutes rather than hours.
- Diagnostic AI is now being integrated into handheld ultrasound devices, allowing a nurse or a paramedic in a rural area to get a "doctor-level" scan of a patient's heart or abdomen in the field.
- The technology is also being used in pathology to analyze tissue slides for cancer, providing a level of "counting" and measuring accuracy that is impossible for a human using a microscope.
Pricing: Hospitals typically pay a subscription fee for AI imaging software, which can range from $2,000 to $10,000 per month per department.
- Some vendors use a "per-scan" model, charging between $5 and $20 for every image that the AI analyzes and reports on.
- Integrated software suites for entire hospital networks can have annual contract values of $250,000 to $1 million, depending on the volume of imaging performed.
Why it matters: Accurate and early diagnosis is the most effective way to save lives and reduce costs. By using AI to catch diseases in their earliest, most treatable stages, we can significantly improve survival rates for cancer and heart disease, which are the leading causes of death in the United States.
11. 5G-Enabled Smart Hospitals and Remote Surgery
The rollout of 5G across the United States has provided the "high-speed backbone" that health technology needs to function at scale. Unlike older Wi-Fi or 4G networks, 5G offers ultra-low latency, meaning there is zero delay between a surgeon's movement and a robotic arm's response. This has made "telerobotic surgery" a reality, where a world-class specialist in a city can operate on a patient in a rural community hospital without any lag. 5G also allows thousands of IoMT devices to be connected in a single building without slowing down the network, creating a truly "smart hospital" environment.
- 5G enables "massive IoT," allowing a hospital to track the real-time location and status of every piece of equipment, from wheelchairs to life-saving ventilators, reducing lost time and equipment waste.
- The high bandwidth allows for the instant transmission of massive 4K medical video and 3D imaging files, which is essential for real-time consultations between different medical teams.
- In ambulances, 5G allows paramedics to transmit a patient's full vital signs and live video to the emergency room staff, so the hospital can be perfectly prepared before the patient even arrives.
- The network supports "edge computing," where data is processed right at the patient's bedside instead of being sent to a distant server, providing instant alerts for critical changes in a patient's condition.
- Smart hospitals use 5G to power autonomous delivery robots that carry medications, linens, and meals through the halls, allowing human staff to stay focused on patient care.
Pricing: Implementing a private 5G network for a hospital campus typically involves an initial investment of $500,000 to $2 million depending on the size of the facility.
- Monthly maintenance and service fees for a managed 5G healthcare network can range from $10,000 to $50,000.
- Individual 5G-enabled medical devices often carry a premium cost of 15% to 20% higher than their Wi-Fi-only counterparts.
Why it matters: 5G is the "connective tissue" that makes all other technologies possible. In a country as large as the US, the ability to transmit high-level medical expertise and data over long distances is the only way to ensure that everyone, regardless of where they live, has access to the best possible healthcare.
12. Blockchain for Secure Healthcare Data Interoperability
One of the biggest problems in American healthcare is "data silos," where your records at one hospital cannot be easily accessed by a doctor at another. Blockchain technology is solving this by creating a secure, decentralized "ledger" of a patient's medical history that is owned and controlled by the patient, not the hospital. This allows for seamless data sharing while maintaining the highest level of security and privacy. In 2026, blockchain is also being used to track the pharmaceutical supply chain, ensuring that every bottle of medicine in the US is authentic and has not been tampered with.
- Patients use "digital keys" to grant temporary access to their medical records to a new doctor, and every time someone views the record, it is permanently logged in a way that cannot be erased or altered.
- The technology automates the complex "prior authorization" process between doctors and insurance companies, using smart contracts to approve treatments instantly if they meet pre-defined medical criteria.
- Blockchain is used to secure clinical trial data, making it impossible for researchers to "cherry-pick" or hide negative results, which improves the overall trust in new medical treatments.
- In the pharmacy space, blockchain tracks every step of a drug's journey from the factory to the patient, which is essential for preventing the $200 billion global trade in counterfeit medications.
- The system allows for "micropayments" and easier billing, as the ledger can automatically verify that a service was performed and trigger an immediate payment from the insurance company to the provider.
Pricing: Integrating a blockchain layer into an existing EHR system typically costs between $50,000 and $150,000 for the initial setup.
- Transaction fees for using a public or semi-private healthcare blockchain are usually very low, often less than $0.05 per data exchange.
- Enterprise supply chain tracking platforms for pharmaceutical companies can cost between $10,000 and $30,000 per month, depending on the volume of products tracked.
Why it matters: Blockchain puts the patient back in control of their own information. By solving the trust and security issues that have plagued healthcare data for decades, it finally makes it possible for a patient's information to follow them wherever they go, leading to safer and more coordinated care.
13. Neurotechnology and Brain-Computer Interfaces (BCI)
Neurotechnology is the science of connecting the human brain directly to computers, and it is moving from experimental trials to real-world medical use. Brain-Computer Interfaces (BCI) can help paralyzed patients regain the ability to speak or move by translating their thoughts into text on a screen or movement in a robotic limb. In the US, companies like Neuralink and Blackrock Neurotech are leading the way in developing implants that can treat severe depression, epilepsy, and even restore some level of sight to the blind. By 2026, these "neural implants" are becoming a recognized treatment option for patients who have exhausted all other medical possibilities.
- BCIs can be "invasive" (implanted in the brain) or "non-invasive" (worn like a cap), depending on the level of precision and the type of medical condition being treated.
- The software uses machine learning to "learn" the unique patterns of a patient's brain, allowing the interface to become faster and more accurate the more the patient uses it.
- Beyond paralysis, neurotechnology is being used to deliver "deep brain stimulation" for Parkinson's disease, which can instantly stop tremors and allow patients to regain control of their bodies.
- New "bioelectronic" medicines use tiny implants to stimulate the vagus nerve, which can treat inflammatory diseases like rheumatoid arthritis without the need for heavy medications.
- Research is currently underway to use BCIs to "download" a patient's memory or cognitive state to help monitor and slow the progression of Alzheimer's disease.
Pricing: The cost of a BCI surgical implantation and the accompanying hardware is currently estimated to be between $100,000 and $250,000.
- Ongoing software maintenance and "brain-training" sessions can cost patients between $1,000 and $3,000 per year.
- Non-invasive neurotech headsets for wellness and focus are available for consumers for $500 to $1,500.
Why it matters: This is the ultimate "quality of life" innovation. For patients who have lost the ability to communicate or move, neurotechnology provides a bridge back to the world, offering a level of independence that was previously unimaginable in the history of medicine.
14. Digital Therapeutics (DTx) and mHealth
Digital Therapeutics are software-based treatments that are "prescribed" by a doctor to treat a medical condition, just like a pill. These are not just "health apps," they are clinically validated platforms that use cognitive behavioral therapy (CBT), gamification, and data tracking to treat conditions like insomnia, substance abuse, and diabetes. In the US, the FDA has created a specific pathway for these products, and many major insurance companies now cover the cost of a "prescription app." This allows for 24/7 support and treatment that can be accessed from the patient's smartphone, making mental and chronic care more accessible.
- DTx programs use "closed-loop" feedback, where the app changes its lessons or challenges based on the patient's daily mood, sleep data, and physical activity levels.
- These platforms often include a "human-in-the-loop" feature, where a health coach or therapist can see the patient's progress and step in with a phone call if they see the patient is struggling.
- For diabetes management, digital therapeutics can automatically adjust a patient's insulin doses (when connected to a pump) or provide real-time nutritional advice based on a photo of the patient's meal.
- The technology is particularly effective for behavioral health, providing patients with "in-the-moment" coping tools when they are experiencing a craving or a panic attack, rather than waiting for their next weekly appointment.
- Because they are software-based, DTx programs can be easily updated with the latest clinical research, ensuring that the patient is always receiving the most modern treatment available.
Pricing: A "prescription" for a digital therapeutic typically costs between $200 and $800 for a 12-week program.
- Some apps operate on a monthly subscription model, ranging from $30 to $150 per month, often with a co-pay from the patient's insurance.
- Many companies offer "employer-sponsored" versions of these tools at a bulk rate of $5 to $15 per employee per month.
Why it matters: Digital Therapeutics solve the problem of "provider shortages." In many parts of the US, there aren't enough therapists or specialists to go around, and these software treatments allow millions of people to get evidence-based care immediately on their own terms.
15. Nanomedicine and Targeted Nano-Delivery
Nanomedicine involves the use of materials at the "nanoscale" (one-billionth of a meter) to diagnose and treat diseases at the cellular level. This technology allows for "smart" drug delivery, where a medication is encased in a tiny nanoparticle that only opens when it reaches a specific target, such as a cancer cell or an area of inflammation. This means that a much smaller amount of medicine is needed, and because it doesn't affect the rest of the body, the side effects are significantly reduced. By 2026, nanomedicine is a primary driver behind the success of new cancer treatments and mRNA-based vaccines in the US.
- Nanoparticles can be engineered to bypass the "blood-brain barrier," allowing for the treatment of brain diseases that were previously unreachable with traditional liquid medications.
- "Nanosensors" can be injected into the bloodstream to look for the earliest signs of disease, such as a single cancer cell or a tiny amount of plaque in an artery, and "report" that data back to a wearable device.
- This technology is being used to create "self-healing" dental fillings and bone grafts that use nanomaterials to encourage the body's natural cells to grow back and repair damage.
- In cancer care, nanomedicine is used to deliver "chemo-bombs" that only release their toxic load inside the tumor, sparing the patient from the hair loss, nausea, and fatigue associated with traditional chemotherapy.
- Research is also exploring "nanobots" that could eventually perform tiny "surgeries" inside a patient's veins, clearing out blockages or repairing damaged tissue from the inside out.
Pricing: Treatments involving nanotechnology are currently high-cost, with specialized infusions ranging from $10,000 to $50,000 per session.
- The laboratory equipment required to manufacture these nanoparticles is extremely expensive, with costs for a facility starting at $2 million to $5 million.
- As the technology scales, the cost of "nano-formulated" versions of common drugs is expected to be 20% to 50% higher than standard versions.
Why it matters: Nanomedicine is the future of "side-effect-free" treatment. By being able to target the disease with surgical precision at the molecular level, we can make the most powerful medicines in the world safer and more effective for everyone.
Showcase Your Expertise with Fueler
In the fast-moving world of healthcare technology, having the right skills is only half the battle, as you also need to show what you can do. Whether you are a software developer building the next great medical SaaS or a healthcare administrator optimizing hospital workflows, your work speaks louder than a bullet point on a resume. Fueler is a skills-first portfolio platform designed to help you document your projects, assignments, and professional achievements in a way that captures the attention of top companies. Instead of telling a recruiter you know how to manage a healthcare database, you can show them the actual system you built or the case study of a successful implementation you led. In a world that is moving away from traditional credentials, Fueler helps you stand out by proving your value through a high-quality, professional portfolio of work.
Final Thoughts
The health technology landscape in the United States for 2026 is defined by a shift from "reactive" medicine to "proactive" and "personalized" care. Innovations like AI, 5G, and genomics are no longer just buzzwords, as they have become the essential tools that keep our hospitals running and our patients healthy. While the costs of some of these breakthroughs remain high, the long-term value they provide by preventing chronic illness and streamlining administration is undeniable. For professionals entering this space, the opportunity to make a real-world impact has never been greater, provided they can prove their expertise through results and documented work. As these technologies continue to converge, we are moving closer to a future where healthcare is not just a service we receive when we are sick, but a continuous part of our daily lives.
Frequently Asked Questions
What are the most significant health tech trends in the US for 2026?
The most significant trends include the widespread adoption of AI-powered medical scribes to reduce doctor burnout, the rise of "Hospital-at-Home" through remote patient monitoring, and the use of generative AI to drastically speed up the discovery of new drugs. These technologies are leading the way because they address the core problems of cost, access, and workforce shortages in the American healthcare system.
How does AI improve medical diagnosis in 2026?
AI improves diagnosis by acting as a highly accurate "second pair of eyes" for doctors, particularly in medical imaging and pathology. It can analyze thousands of X-rays or tissue slides in seconds, spotting tiny abnormalities that the human eye might miss and flagging urgent, life-threatening cases so they can be treated immediately in the emergency room.
Is remote surgery safe and available in the United States?
Yes, remote surgery is becoming increasingly safe thanks to the rollout of 5G networks, which provide the ultra-low latency (zero delay) required for a surgeon to control a robotic arm from a different city. While it is still used primarily for specialized or emergency cases where a local expert is not available, it is a rapidly growing field that is improving access to care for rural Americans.
What is the cost of a typical gene-editing treatment?
Currently, FDA-approved gene-editing treatments like CRISPR are among the most expensive medical procedures in history, often costing between $2 million and $3 million per patient. However, because these are designed as "one-time cures" for chronic genetic diseases, insurance companies are beginning to see them as a cost-effective alternative to a lifetime of expensive medications and hospital stays.
Can patients own and control their own medical data?
Through the use of blockchain technology and new federal regulations, patients are gaining much more control over their own medical records. In 2026, many Americans are using digital "health wallets" that allow them to securely store their own data and grant temporary access to any doctor or specialist they choose, ensuring that their medical history is always available when they need it.
What is Fueler Portfolio?
Fueler is a career portfolio platform that helps companies find the best talent for their organization based on their proof of work. You can create your portfolio on Fueler. Thousands of freelancers around the world use Fueler to create their professional-looking portfolios and become financially independent. Discover inspiration for your portfolio
Sign up for free on Fueler or get in touch to learn more.