Top 15 Health Tech Platforms Used by US Hospitals in 2026

Riten Debnath
15 Jan, 2026

The modern American hospital is no longer just a building of brick and mortar; it is a sophisticated data center where software platforms dictate the speed of care and the precision of surgery. In 2026, the "best" platforms are those that bridge the gap between administrative necessity and clinical excellence, ensuring that patient data flows securely from an ambulance to an operating room without friction. For hospital administrators, choosing the right tech stack is a high-stakes decision that impacts everything from multi-million dollar revenue cycles to the daily mental health of their nursing staff.
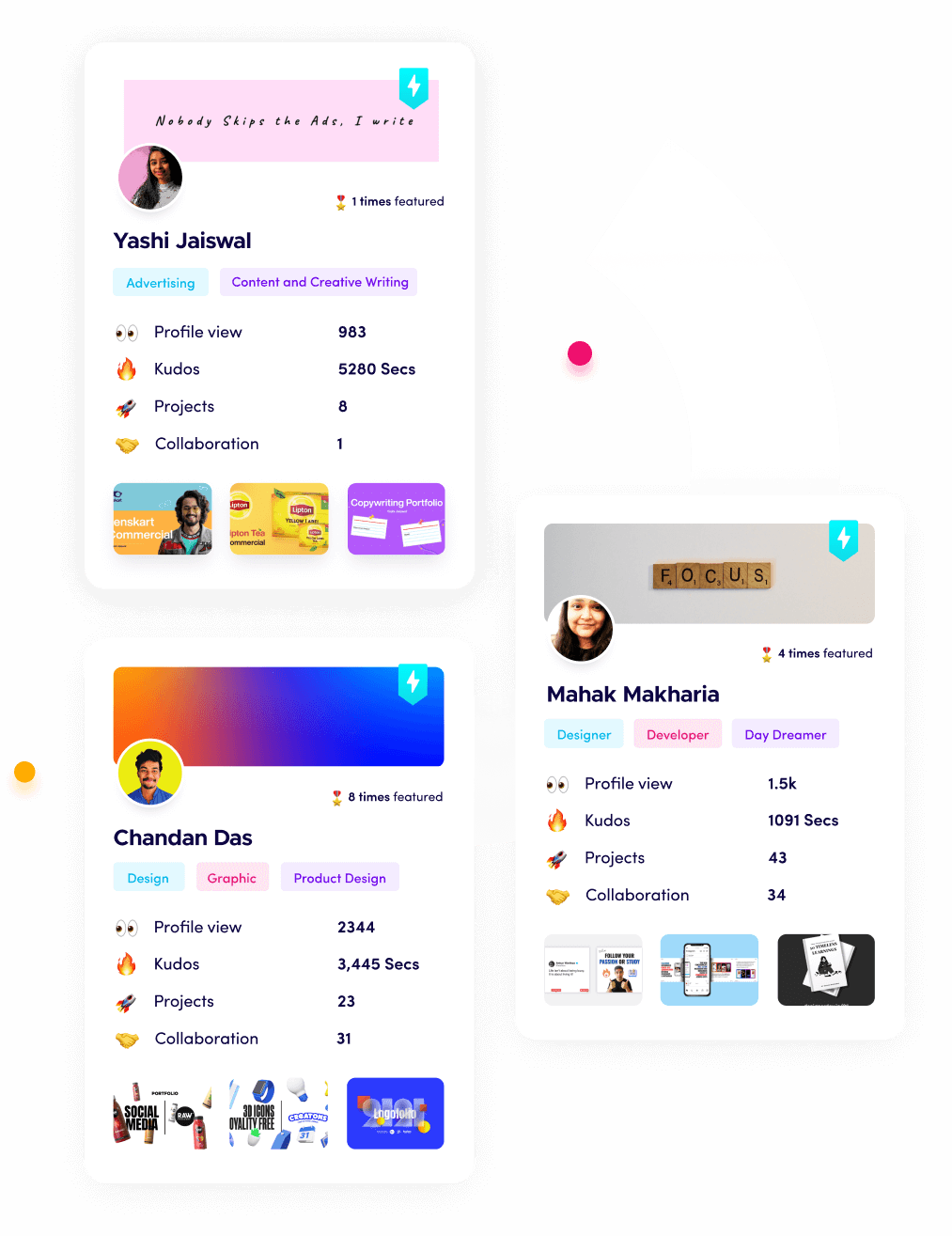
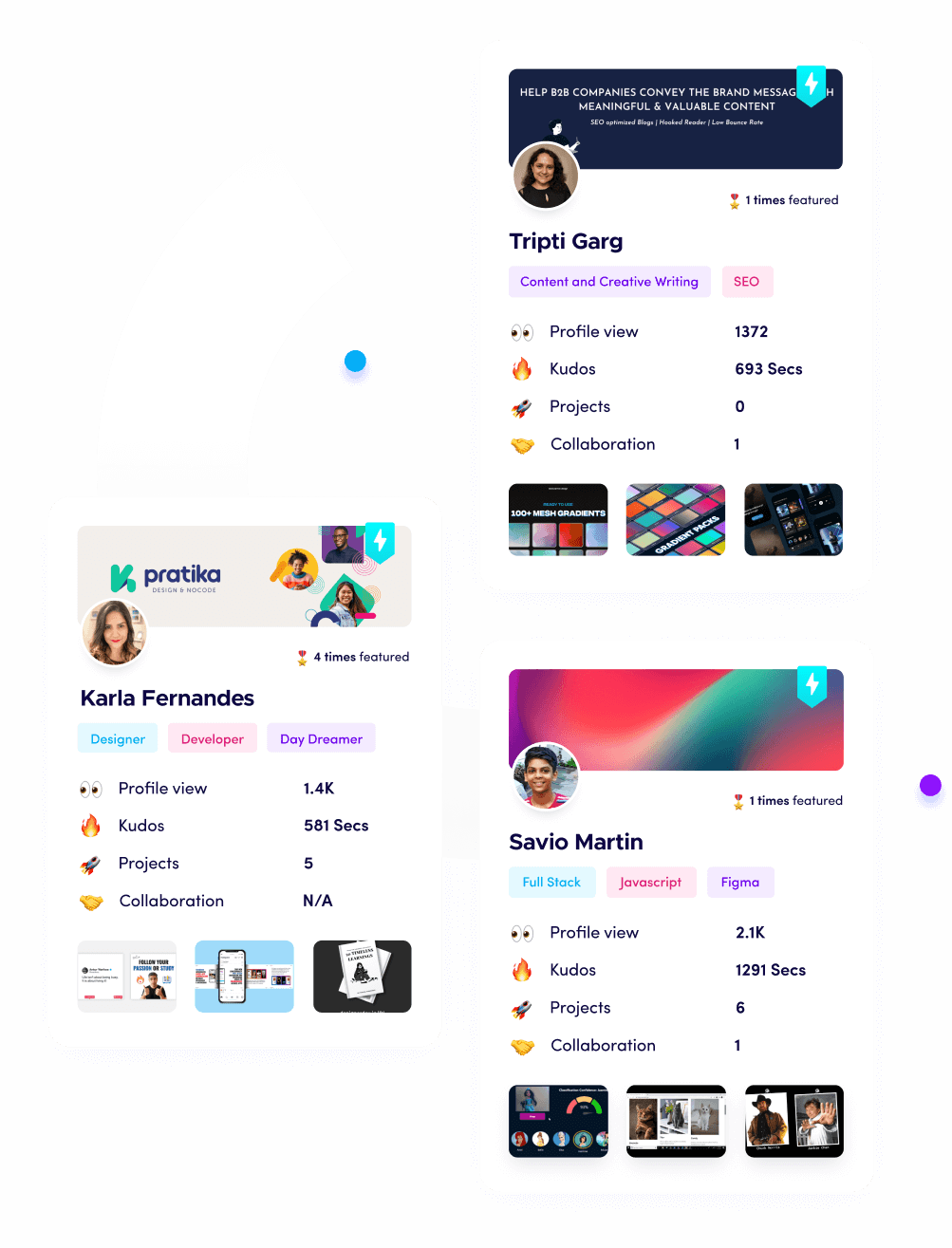
I’m Riten, the founder of Fueler - a skills-first portfolio platform that connects talented individuals with companies through assignments, portfolios, and projects, not just resumes/CVs. Think Dribbble/Behance for work samples + AngelList for hiring infrastructure.
1. Epic Hyperdrive (Enterprise EHR)
Epic Hyperdrive is the web-based evolution of the world's most powerful electronic health record system, designed to handle the massive data loads of Tier-1 trauma centers and university hospitals. By moving away from legacy desktop clients, Hyperdrive allows clinicians to access patient records through any secure browser, providing a faster, more responsive interface that supports complex workflows like genomic mapping and transplant coordination. Its dominance in the US market ensures that it remains the primary "operating system" for over half of all American hospital beds.
- Hyperdrive Web-Based Infrastructure: The shift to a browser-based environment allows hospital IT departments to deploy updates instantly across thousands of workstations without the need for manual installations, significantly reducing the downtime that traditionally plagued large-scale hospital software upgrades.
- Cosmos Global Data Insights: This integrated research network allows clinicians to query the de-identified health data of over 200 million patients in real-time, providing immediate evidence-based guidance for treating rare conditions or predicting how a specific patient might react to a new medication.
- Lumos Predictive Analytics: Integrated directly into the clinical workflow, Lumos uses machine learning to alert care teams about patients at high risk for sepsis or sudden cardiac arrest hours before traditional vital signs would indicate a problem, effectively saving lives through early intervention.
- Epic Cheers CRM Integration: This module transforms the EHR into a patient-relationship powerhouse, allowing hospitals to manage outreach campaigns for preventive screenings and follow-ups as efficiently as a retail business, ensuring that no patient "falls through the cracks" of the care continuum.
- Garden Plot for Independent Groups: Recognizing the need for interoperability, Epic now offers a hosted version for smaller, independent physician groups that work within larger hospital networks, allowing for a seamless flow of data between primary care doctors and hospital-based specialists.
Pricing:
- Enterprise implementations typically start at $10 million to $50 million for initial setup.
- Ongoing annual maintenance and licensing fees usually range from $2 million to $5 million, depending on the number of active users and modules.
2. Oracle Health Millennium (Cloud-Native EHR)
Following Oracle’s acquisition of Cerner, the Millennium platform has been completely re-engineered as a cloud-native solution that leverages Oracle’s Tier-4 data centers for unmatched reliability. In 2026, Millennium was favored by large multi-state health systems and the Department of Veterans Affairs for its ability to handle massive, distributed datasets. The platform’s newest iterations focus on "Zero-Click Documentation," using ambient sensors to record patient encounters so that doctors can spend their time making eye contact instead of typing.
- Oracle Cloud Infrastructure (OCI) Migration: By moving to a dedicated healthcare cloud, Millennium has achieved near-zero latency, ensuring that critical patient data like high-resolution imaging and real-time telemetry is available to surgeons the millisecond it is captured in the diagnostic lab.
- Clinical AI Voice Assistant: The platform features an integrated voice-activated agent that allows clinicians to update charts, order labs, and check medication dosages through simple verbal commands, effectively acting as a digital scribe that lives within the hospital's secure wireless network.
- HealtheIntent Population Analytics: This proactive tool aggregates data from multiple sources, including pharmacies and social service agenciesto give hospital administrators a holistic view of community health trends, allowing them to allocate resources to neighborhoods facing specific health crises.
- Seamless Pharmacy & Supply Integration: Millennium connects directly to the hospital’s automated pharmacy dispensers and surgical supply chains, triggering automatic reorders the moment a medication is scanned at the bedside or a stent is used in the cardiac catheterization lab.
- Command Center Dashboard: This executive-level interface provides a "bird's-eye view" of hospital operations, tracking everything from emergency room wait times to the current availability of intensive care beds across an entire regional network of medical facilities.
Pricing:
- Mid-to-large hospital systems can expect annual subscription costs starting at $1.5 million to $4 million.
- Custom enterprise contracts for large-scale federal or multi-state deployments often exceed $100 million over a ten-year period.
3. Microsoft Cloud for Healthcare (Infrastructure & Collaboration)
Microsoft has become an indispensable layer of the hospital tech stack by providing the secure "connective tissue" between different medical applications through Azure and Teams. In 2026, Microsoft Cloud for Healthcare is the platform of choice for hospitals looking to unify their communication, data storage, and AI development under a single HIPAA-compliant umbrella. It serves as the foundation upon which many other healthtech tools are built, offering specialized AI models for medical imaging and natural language processing.
- Teams for Care Coordination: Far more than a chat app, Teams in a hospital setting serves as a secure "war room" where multidisciplinary teams can view a patient's EHR data, lab results, and imaging while discussing treatment plans in a protected, encrypted environment.
- Azure Health Data Services: This specialized cloud service allows hospital IT teams to ingest and normalize data from diverse sources like wearables, medical devices, and legacy software, making it available for advanced research and real-time clinical decision support.
- Nuance DAX Copilot Integration: Microsoft’s integration of Nuance’s ambient listening technology allows for the automatic generation of clinical notes during patient visits, which are then reviewed and signed by the physician, drastically reducing the administrative burden on hospital staff.
- Healthcare-Specific AI Models: Through Azure, hospitals can access pre-trained AI models specifically designed to identify anomalies in X-rays, summarize long medical histories, and even predict patient no-show rates to help optimize the clinic's daily schedule.
- Secure Patient Outreach Tools: The platform includes sophisticated automation for patient engagement, allowing hospitals to send personalized health reminders and educational content via secure email or SMS, increasing patient adherence to long-term treatment plans.
Pricing:
- Licensing for the Healthcare Add-on typically starts at $95 per user per month for smaller facilities.
- Enterprise agreements for large hospital networks often range from $500,000 to $2 million per year, depending on data storage and AI usage.
4. Meditech Expanse (EHR for Community Hospitals)
Meditech Expanse has carved out a massive niche by providing a high-end, mobile-first EHR experience specifically designed for community and regional hospitals that may not have the budget for Epic. In 2026, Expanse was praised for its intuitive, "app-like" interface that requires significantly less training than its competitors. It offers a "Full-Circle" care model, ensuring that the patient's data follows them from the emergency room to the surgical suite and eventually back to their primary care physician.
- Mobile-First Clinician Experience: The platform is built natively for tablets and smartphones, allowing doctors and nurses to view charts and enter data while standing at the bedside or walking through the halls, rather than being tethered to a bulky computer on wheels.
- Integrated Precision Medicine: Expanse includes built-in genomic tools that allow clinicians to see how a patient’s DNA might impact their response to certain medications, bringing high-end specialized care to smaller community hospitals that were previously priced out of such tech.
- Expanse Patient Connect: This integrated portal allows patients to check in for appointments remotely, pay bills, and communicate with their care team, all through a modern interface that mirrors the ease of use found in consumer banking or travel apps.
- High-Performance Revenue Cycle: Meditech’s billing and financial modules are deeply integrated into the clinical workflow, ensuring that every procedure and medication is accurately captured for billing purposes, which helps smaller hospitals maintain thin profit margins.
- Trauma and Emergency Modules: The platform includes specialized workflows for high-pressure environments like the ER, providing clinicians with "at-a-glance" status boards and rapid-entry tools that prioritize speed without sacrificing the accuracy of the medical record.
Pricing:
- Implementation for mid-sized community hospitals usually starts around $1 million to $3 million.
- Monthly subscription and support fees typically range from $25,000 to $60,000 for the entire facility.
5. GE HealthCare Centricity (Imaging & Cardiology)
While often known for its physical MRI and CT machines, GE HealthCare’s Centricity platform is the leading software for managing the massive files generated by hospital imaging departments. In 2026, Centricity has evolved into an AI-driven "Intelligence Platform" that helps radiologists spot tiny fractures or early-stage tumors that might be missed by the human eye. It serves as the primary archive for all visual medical data, ensuring that a patient’s scans from five years ago are instantly accessible for comparison.
- Centricity Universal Viewer: This high-speed viewing platform allows radiologists to access and analyze images from any department/radiology, cardiology, or pathology within a single interface, eliminating the need to log into multiple disparate systems to see a patient's full visual history.
- AI-Assisted Diagnostic Triage: The platform automatically scans incoming images and "flags" those that show urgent issues like a brain hemorrhage or collapsed lung, moving them to the top of the radiologist's worklist to ensure life-saving treatment begins immediately.
- Enterprise Imaging Archive: GE provides a massive, scalable storage solution that can handle petabytes of medical images, ensuring that hospitals remain compliant with long-term data retention laws while keeping the data "warm" and accessible for instant retrieval.
- Advanced Cardiology Workflow: The Centricity Cardio Enterprise module provides specialized tools for heart surgeons and cardiologists, integrating ECG data, ultrasound videos, and surgical reports into a single, cohesive view of the patient’s cardiovascular health.
- Interoperable Data Sharing: The platform uses the latest FHIR and DICOM standards to ensure that medical images can be sent securely to other hospitals or specialists across the country, preventing the need for patients to carry physical CDs of their medical scans.
Pricing:
- Enterprise imaging suites are typically quoted based on volume, with initial setups starting at $500,000.
- Annual maintenance and cloud storage fees usually range from $100,000 to $300,000, depending on the size of the imaging department.
6. Athenahealth (Ambulatory and Network Management)
Athenahealth is the leading cloud-native platform for outpatient clinics and hospital-owned physician networks. In 2026, it is famous for its "athenaOne" suite, which combines EHR, medical billing, and patient engagement into a single ecosystem that is continuously updated in the cloud. Unlike legacy systems, Athenahealth takes a proactive role in a hospital's financial health, using its massive network data to identify why certain insurance claims are being denied and automatically fixing them before they are even sent.
- Network-Driven RCM Intelligence: Athenahealth monitors the billing patterns of thousands of clinics across the US, using that data to create a "rules engine" that ensures a hospital’s claims are perfectly formatted to meet the ever-changing requirements of private and government insurance payers.
- AthenaTelehealth Integration: The platform features a built-in virtual care solution that allows doctors to launch video visits directly from the patient’s chart, ensuring that the documentation and billing for the remote visit happen automatically in the background.
- Epocrates Clinical Decision Support: Integrated directly into the prescribing workflow, this tool provides clinicians with instant information on drug interactions, pill identification, and the latest clinical guidelines, ensuring that every prescription is safe and evidence-based.
- Automated Patient Outreach: Athenahealth’s engine automatically sends text and email reminders to patients for upcoming appointments, lab results, and overdue screenings, which significantly reduces "no-show" rates and improves overall community health outcomes.
- Specialty-Specific Workflows: The platform offers customized clinical templates for over 50 medical specialties, from pediatrics to oncology, ensuring that doctors don't have to scroll through irrelevant data fields to find the information they need for their specific practice area.
Pricing:
- Athenahealth typically uses a "percentage of collections" model, usually ranging from 4% to 7% of a practice’s monthly revenue, aligning their success with the hospital's financial performance.
- There are often no massive upfront "licensing" fees, making it an attractive "SaaS" model for growing health networks.
7. Salesforce Health Cloud (Patient Experience CRM)
Salesforce Health Cloud has become the standard for "Patient Relationship Management," allowing hospitals to treat patients as individuals rather than just medical record numbers. In 2026, it is used by major US health systems to coordinate care across multiple facilities, track patient satisfaction, and manage large-scale clinical trials. By sitting on top of the traditional EHR, Health Cloud provides a 360-degree view of the patient's life, including social determinants of health like their access to transportation or healthy food.
- 360-Degree Patient Profile: This interface consolidates data from the EHR, insurance records, and even wearable devices to give care coordinators a complete picture of a patient’s health journey, including their preferences for communication and their history of engagement.
- Automated Care Plans: Health Cloud allows hospitals to build standardized digital "journeys" for patients with chronic conditions like diabetes, automatically triggering reminders, educational videos, and check-in calls based on the patient's real-time progress.
- Referral Management Engine: The platform streamlines the process of sending patients to specialists, ensuring that the receiving doctor has all the necessary clinical data and that the hospital can track whether the patient actually attended the follow-up appointment.
- Social Determinants of Health (SDoH) Tracking: Salesforce allows clinicians to log non-medical factorssuch as housing instability or food insecuritythat might impact a patient’s recovery, allowing the hospital to connect them with social workers or community resources.
- Clinical Trial Management: For academic medical centers, Health Cloud provides a robust platform for recruiting and tracking participants in clinical trials, ensuring that all regulatory requirements are met while keeping patients engaged throughout the study.
Pricing:
- Health Cloud Enterprise Edition typically starts at $300 per user per month, though hospitals usually negotiate large-volume discounts.
- Professional services for implementation and customization can range from $100,000 to over $1 million for complex hospital systems.
8. Philips HealthSuite (Connected Care & Monitoring)
Philips HealthSuite is an integrated cloud platform that connects a hospital’s bedside monitors, ventilators, and wearable sensors into a single data stream. In 2026, it is the premier tool for "High-Acuity Care," allowing a single nurse in a centralized "Command Center" to monitor the vitals of dozens of patients across different floors or even different hospitals. This "Tele-ICU" capability is essential for managing nursing shortages while ensuring that critically ill patients receive constant, expert oversight.
- eICU Program Connectivity: The platform allows world-class intensive care doctors to virtually "step into" any patient room via high-definition video and real-time data feeds, providing expert guidance to on-site staff during emergencies regardless of their physical location.
- Predictive Patient Deterioration Alerts: Using its "IntelliVue" algorithms, HealthSuite analyzes trends in heart rate, oxygen levels, and blood pressure to predict when a patient is likely to experience a "code blue" event up to six hours before it happens.
- Interoperable Medical Device Integration: Philips provides the "middleware" that allows medical devices from many different manufacturers to "talk" to the hospital’s main EHR, ensuring that vitals are recorded automatically and accurately without manual transcription.
- Hospital-to-Home Transition Tools: The platform includes remote monitoring kits that patients take home after surgery, allowing the hospital to track their recovery and intervene via telehealth if their vitals show signs of infection or other complications.
- Operational Performance Analytics: HealthSuite provides administrators with detailed reports on how medical equipment is being used across the facility, identifying "ghost assets" that are sitting idle and helping the hospital optimize its multi-million dollar equipment budget.
Pricing:
- Implementation for a 200-bed hospital typically starts at $750,000.
- Annual "Connected Care" subscriptions usually cost between $150,000 and $400,000 depending on the number of monitored beds and the depth of AI analytics used.
9. Infor CloudSuite Healthcare (ERP & Supply Chain)
While other platforms focus on the patient, Infor CloudSuite Healthcare focuses on the "business" of the hospital, managing the staff, the supplies, and the finances. In 2026, it is the most widely used Enterprise Resource Planning (ERP) system in the US medical sector. It ensures that when a surgeon needs a specific type of heart valve, it is in stock, and when a nurse works overtime, they are paid correctly and on time according to complex union and federal regulations.
- Healthcare-Specific Supply Chain: Infor’s system is designed to handle the complexities of medical inventory, including tracking expiration dates on expensive medications and managing the "recall" process for faulty medical devices across an entire hospital network.
- Strategic Human Capital Management: The platform manages the credentials, licenses, and scheduling for thousands of healthcare workers, automatically alerting administrators if a nurse’s license is about to expire or if a shift is dangerously understaffed.
- Financial Integrated Management: Infor consolidates the hospital’s various revenue streams from gift shop sales to multi-million dollar insurance payouts into a single financial record, providing real-time "profit and loss" statements for every department in the building.
- AI-Powered Demand Forecasting: The system analyzes years of hospital data to predict when the facility will see a surge in patients (such as during flu season), allowing the supply chain team to pre-order extra masks, gowns, and medications before prices spike.
- Clinical Bridge Integration: Unlike generic business software, Infor includes a "Clinical Bridge" that allows it to pull data from the EHR, ensuring that the supplies used during a surgery are automatically deducted from inventory and added to the patient’s bill.
Pricing:
- Enterprise contracts for large health systems usually range from $2 million to $5 million per year.
- Implementation costs are high, often requiring a $1 million to $3 million investment in professional services to map the hospital's complex workflows.
10. TigerConnect (Clinical Communication & Collaboration)
TigerConnect is the primary "secure messaging" platform used in US hospitals to replace outdated pagers and unencrypted text messages. In 2026, it became a full-scale "Collaboration Platform" that integrates directly with the hospital’s on-call schedule and EHR. It ensures that when a nurse needs to reach the on-call neurologist at 3 AM, they don't have to look up a phone number; they simply message the "Neurology Role," and the system automatically routes the message to the correct person.
- Role-Based Messaging Logic: Instead of searching for individuals, staff send messages to "roles" (e.g., "Charge Nurse 4th Floor"), ensuring that critical information always reaches the person currently on duty regardless of shift changes or staff turnover.
- EHR-Integrated Patient Context: When a clinician discusses a patient in TigerConnect, they can "attach" a snippet of the patient’s record or a lab result, ensuring that everyone in the conversation has the full clinical context without leaving the secure app.
- Alarm Management & Fatigue Reduction: The platform integrates with bedside monitors to send "critical alerts" directly to a nurse’s smartphone, but it uses AI to filter out "nuisance alarms," reducing the "alarm fatigue" that often leads to staff burnout and missed emergencies.
- Secure Video and Image Sharing: Doctors can take high-resolution photos of wounds or rashes and share them securely with specialists for an instant second opinion, with the photos being stored in the secure TigerConnect cloud rather than on the doctor's personal device.
- External Community Collaboration: The platform allows hospital staff to securely message doctors in the community, home health nurses, and even patients, creating a "unified circle of care" that extends far beyond the physical walls of the hospital building.
Pricing:
- Standard clinical tiers typically start at $10 to $15 per user per month.
- Enterprise-wide hospital deployments with full EHR and alarm integration usually range from $100,000 to $250,000 per year, depending on the facility size.
11. DrChrono (Customizable EHR and Practice Management)
DrChrono is a favorite among innovative hospitals and ambulatory surgical centers that prioritize an "iPad-first" workflow and deep customization. In 2026, it is particularly popular for its "open API," which allows hospital IT teams to build their own custom apps on top of the medical record. It is frequently used by specialized clinics, such as orthopedics or plastic surgery, within larger hospital systems that require more flexible documentation templates than a "one-size-fits-all" enterprise EHR can provide.
- iPad Native Clinical Workflow: DrChrono was built from the ground up for the iPad, offering a tactile, gesture-based interface that allows clinicians to draw on anatomical diagrams and dictate notes with extreme speed and fluidity during a patient encounter.
- Highly Customizable Form Builder: Hospitals use DrChrono to create specialized medical forms that mirror their specific paper workflows, ensuring that clinicians don't have to change the way they practice medicine to fit the requirements of the software.
- Integrated Billing and RCM Suite: The platform includes an end-to-end medical billing solution that handles everything from initial insurance eligibility checks to final patient collections, with a "real-time" dashboard that tracks the financial health of the clinic.
- Open API for Third-Party Apps: DrChrono features one of the most robust "App Stores" in the medical industry, allowing hospitals to plug in third-party tools for things like AI-driven heart monitoring or automated patient check-in kiosks with a single click.
- Patient Portal and Check-in Kiosk: The system includes a modern patient portal where users can fill out "digital clipboards" on their own devices before they arrive, significantly reducing waiting room times and eliminating manual data entry for front-desk staff.
Pricing:
- The "Prometheus" tier (highest level) typically starts around $500 per provider per month.
- Enterprise hospital contracts are custom-quoted, usually involving a base licensing fee plus an implementation fee of $50,000 to $150,000.
12. Phreesia (Patient Intake & Financial Engagement)
Phreesia is the "Digital Front Door" that greets millions of patients as they enter US hospitals and clinics. In 2026, it replaced the traditional paper clipboard with a seamless, mobile-first intake process. It handles everything from verifying insurance in real-time to collecting co-pays and screening for social needs. By automating the "boring" parts of the doctor's visit, Phreesia allows hospital staff to focus on providing a warm, human welcome to patients who are often stressed or in pain.
- Mobile Pre-Registration & Intake: Patients receive a secure link before their appointment that allows them to complete all their paperwork, upload a photo of their insurance card, and pay their co-pay from their own couch, drastically reducing congestion in hospital lobbies.
- Real-Time Eligibility Verification: Phreesia’s engine automatically checks a patient’s insurance status the moment they check in, alerting the hospital staff if a plan is inactive or if a specific procedure requires a "prior authorization" from the insurance company.
- Patient Advocacy & Screening Tools: The platform includes standardized screenings for mental health, food insecurity, and fall risks, automatically flagging high-risk patients for the clinical team and providing the patient with relevant community resources based on their answers.
- Post-Visit Engagement & Feedback: After a patient leaves the hospital, Phreesia sends automated follow-up messages to collect satisfaction data and remind the patient of their "next steps," such as scheduling a follow-up or picking up a new prescription.
- Point-of-Service Collections: By providing patients with clear, transparent information about their financial responsibility and offering flexible "payment plans," Phreesia helps hospitals collect more of their revenue upfront while reducing the "billing surprises" that frustrate patients.
Pricing:
- Subscription fees are typically based on patient volume, with mid-sized clinics paying between $300 and $800 per month.
- Large hospital deployments are usually custom contracts ranging from $200,000 to $500,000 annually, often including specialized hardware like "Phreesia Pads."
13. Symplr (Governance, Risk, and Compliance)
In the highly regulated world of US healthcare, Symplr is the platform that ensures every hospital remains "audit-ready" and compliant with federal laws. In 2026, it is the primary tool for managing physician credentials, tracking workplace safety incidents, and ensuring that the hospital’s various software systems meet strict cybersecurity standards. It provides a "single source of truth" for the hospital’s legal and administrative teams, helping them navigate the complex web of Joint Commission and CMS requirements.
- Unified Provider Credentialing: Symplr automates the incredibly complex process of verifying a doctor's medical license, education, and malpractice history, ensuring that only qualified and vetted professionals are allowed to treat patients within the hospital's walls.
- Incident & Safety Management: The platform provides a secure, anonymous way for staff to report "near-miss" medical errors or workplace safety concerns, allowing the hospital to identify dangerous patterns and implement corrective actions before an actual injury occurs.
- Contract and Spend Management: Symplr helps hospital executives track thousands of vendor contracts, from laundry services to medical device leases, ensuring that the hospital is getting the best possible pricing and that no critical contracts expire unexpectedly.
- Workforce Scheduling & Pay Equity: The system includes sophisticated tools for managing nurse schedules, ensuring that staffing levels meet state laws while also providing data to ensure that pay is equitable and compliant with labor regulations across the facility.
- Regulatory & Audit Readiness: Symplr maintains a real-time "Compliance Dashboard" that tracks the hospital's adherence to thousands of different regulatory standards, allowing administrators to prepare for a surprise inspection from the Department of Health in minutes instead of weeks.
Pricing:
- Enterprise modules are typically priced individually, with a full "GRC" (Governance, Risk, and Compliance) suite for a hospital system starting at $500,000 to $1 million per year.
- Smaller specialty modules, such as "Credentialing," can start at $50,000 annually.
14. Wolters Kluwer UpToDate (Clinical Decision Support)
UpToDate is the "Google for Doctors," but with a level of scientific rigor that no general search engine can match. In 2026, it will be integrated directly into the EHRs of almost every major US hospital. When a doctor is faced with a complex case, they turn to UpToDate for the latest, peer-reviewed treatment protocols and diagnostic evidence. It is updated thousands of times per day by a global team of specialists, ensuring that the care provided in a small rural hospital is just as cutting-edge as the care provided at Harvard or Stanford.
- Evidence-Based Treatment Pathways: The platform provides clinicians with clear, step-by-step "decision trees" for treating over 12,000 different medical conditions, based on the very latest clinical research and international medical consensus.
- Integrated Patient Education Leaflets: UpToDate allows doctors to instantly print or email high-quality, easy-to-understand educational materials for patients, ensuring that they leave the hospital with a clear understanding of their diagnosis and their recovery plan.
- Drug Interaction and Dosing Tools: Through its integration with Lexicomp, UpToDate provides an incredibly powerful database of medication information, allowing doctors to check for "hidden" drug interactions and calculate precise dosages for pediatric or elderly patients.
- CME Credit Automation: As doctors use the platform to research patient cases, the system automatically tracks their activity and awards "Continuing Medical Education" (CME) credits, helping them maintain their medical licenses with zero extra paperwork.
- Specialized Lab Interpretation: The platform helps clinicians make sense of complex or unusual lab results, providing context on what a specific "high" or "low" value might mean within the context of the patient’s overall symptoms and medical history.
Pricing:
- Individual physician subscriptions start at $589 per year.
- Institutional hospital-wide licenses are typically custom-quoted, often ranging from $50,000 to $250,000 annually, depending on the number of beds and clinicians served.
15. Zocdoc (Scheduling and Market Presence)
While Phreesia manages patients once they arrive, Zocdoc is the platform hospitals use to find new patients and fill empty appointment slots. In 2026, Zocdoc has become a critical part of the hospital’s "growth strategy," allowing them to capture the "on-demand" patient demographic that wants to book a specialist visit as easily as they would a table at a restaurant. It integrates with most major hospital EHRs, ensuring that when a patient books on Zocdoc, the appointment appears instantly in the hospital’s master schedule.
- Real-Time "Verified" Appointment Booking: Zocdoc connects directly to the hospital’s calendar to show patients only the slots that are truly available, allowing them to book a visit 24/7 without ever having to sit on hold with a call center.
- Insurance Matching Engine: The platform’s sophisticated search engine allows patients to filter for doctors who are "in-network" for their specific insurance plan, reducing the administrative burden on the hospital to verify insurance later in the process.
- Patient Reviews and Transparency: Zocdoc provides a platform for verified patients to leave reviews, helping hospitals build their online reputation and providing prospective patients with the social proof they need to choose a specific surgeon or specialist.
- Automated Waitlist Management: If a patient cancels an appointment at the last minute, Zocdoc automatically notifies other patients who were looking for that specific time, ensuring that the hospital’s expensive specialized equipment and staff time never go to waste.
- "Digital Front Office" Branding: For large hospital systems, Zocdoc provides a branded experience that showcases their entire network of providers, making it easy for a patient to stay within the same health system for all their various medical needs.
Pricing:
- Zocdoc traditionally uses a "per-booking" model, charging hospitals a fee (often around $35 to $110) for each new patient who finds them through the platform.
- There is typically an annual "subscription" or "listing" fee that varies based on the number of providers being featured on the site.
Leverage These Tools for Your Portfolio on Fueler
The healthcare industry is unique because it requires professionals to be masters of both human care and high-stakes technology. Whether you are a project manager who implemented Epic Hyperdrive at a regional hospital, a developer who built a custom API for DrChrono, or a nurse leader who optimized TigerConnect workflows to reduce alarm fatigue, these are massive career milestones. On Fueler, you can document these specific "Proof of Work" achievements in a way that a standard resume never could. By showcasing your hands-on experience with these 15 industry-leading platforms, you position yourself as a highly valuable asset in the competitive US healthtech market.
Final Thoughts
The 15 platforms listed here represent the absolute "frontier" of medical technology in 2026. They are the tools that allow a modern hospital to function as a unified, intelligent organism. As healthcare continues to move toward a "value-based" model where providers are paid for patient outcomes rather than the number of tests they run, these platforms will only become more critical. By understanding the pricing, capabilities, and strategic importance of these tools, you are better equipped to lead the next wave of digital transformation in American medicine.
Frequently Asked Questions
How do US hospitals manage to keep data secure across all these different platforms? Every platform used in a medical setting must strictly adhere to HIPAA (Health Insurance Portability and Accountability Act) regulations, which govern the privacy and security of health data. In 2026, these companies will use enterprise-grade encryption, SOC 2 Type II compliance, and multi-factor authentication to ensure that even when data is shared between systems like Epic and Salesforce, it remains within a "closed loop" that is virtually impenetrable to unauthorized users.
Do these platforms "talk" to each other, or is the data still siloed in 2026?
We have seen a massive push toward interoperability using the FHIR (Fast Healthcare Interoperability Resources) standard. While silos still exist, platforms like Microsoft Cloud for Healthcare and Oracle Health act as translators, allowing once-incompatible systems to share lab results, imaging, and prescriptions in real-time, which significantly reduces the risk of medical errors during patient transfers.
Why is the pricing for these hospital tools so high compared to regular business software?
The cost reflects the extreme liability, regulatory overhead, and specialized engineering required for "mission-critical" software where a system crash could literally cost a life. Furthermore, implementation costs include thousands of hours of training for medical staff and the "mass customization" required to fit the unique clinical workflows of a 500-bed hospital versus a 50-bed rural clinic.
Can a small hospital realistically use the same tools as a giant university system?
Yes, but usually through different "delivery models." While a giant system might host Epic on their own private servers, a smaller community hospital will likely use a hosted version like Meditech Expanse or Athenahealth. These "SaaS" (Software as a Service) models allow smaller facilities to access high-end AI diagnostics and patient portals without needing a 100-person in-house IT department.
How does mastering these platforms benefit my career on Fueler?
In the healthcare sector, "soft skills" aren't enough; you need technical proof of competency. By showcasing a project on Fuelers such as "Optimized Revenue Cycle for a mid-sized clinic using Athenahealth, "you provide a tangible Proof of Work that proves to recruiters you understand both the software and the high-stakes compliance environment of the US medical economy.