Top 7 AI Use Cases in Mental Health in the USA (2026)

Riten Debnath
20 Jan, 2026

In 2026, the intersection of technology and psychology has reached a fever pitch. In the USA, a staggering 1 in 5 adults live with a mental health condition, but the shortage of human providers has left millions without immediate care. This is where Artificial Intelligence steps in not as a replacement for human empathy, but as a 24/7 bridge that ensures no one has to suffer in silence. From predicting a crisis before it happens to providing instant, non-judgmental therapy sessions, AI is fundamentally rewriting the script for mental wellness across the country.
I’m Riten, founder of Fueler, a skills-first portfolio platform that connects talented individuals with companies through assignments, portfolios, and projects, not just resumes/CVs. Think Dribbble/Behance for work samples + AngelList for hiring infrastructure
1. Generative AI "Always-On" Virtual Therapists
The most visible shift in 2026 is the rise of Generative AI companions that provide immediate emotional support. Unlike the clunky chatbots of the past, these modern systems use advanced Large Language Models (LLMs) to hold natural, empathetic conversations. They are specifically trained on Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) frameworks, allowing them to guide users through anxiety spikes or depressive episodes at 3:00 AM when a human therapist is unavailable.
- Dynamic Conversational Continuity: These AI tools remember past sessions and emotional triggers, allowing for a long-term therapeutic relationship that evolves with the user’s personal growth.
- Non-Judgmental Safe Spaces: Many US users report feeling more comfortable sharing deep-seated traumas with an AI first, as it removes the fear of human social stigma or bias.
- Evidence-Based Skill Drills: The AI can lead users through interactive exercises, such as "graded exposure" for social anxiety or "box breathing" for panic attacks, in real-time.
- Clinical Triage Integration: If the AI detects specific "red flag" language or high-risk sentiment, it can instantly escalate the case to a human emergency professional or a crisis hotline.
- Affordable Accessibility: These tools provide a low-cost alternative for the millions of Americans who are underinsured or live in "provider deserts" where therapy is too expensive or distant.
Why it matters:
With the US facing a critical shortage of over 4.5 million mental health providers, virtual therapists provide a scalable solution. They act as a front-line defense, ensuring that low-to-medium risk individuals receive support while freeing up human doctors for the most complex clinical cases.
2. Predictive Analytics for Crisis Prevention
In 2026, AI is moving from being reactive to being proactive. By analyzing "digital biomarkers" from smartphones and wearable devices, AI models can now predict a mental health decline weeks before it actually happens. These systems look for subtle changes in sleep patterns, heart rate variability, and even the speed of typing or social media usage to identify if someone is drifting toward a depressive episode or a manic state.
- Digital Phenotyping: This involves the continuous monitoring of a user's interaction with their phone to detect behavioral shifts that indicate a change in mental state.
- Suicide Risk Detection: Advanced algorithms now analyze social media posts and private journals with over 90% accuracy to identify patterns of "hopelessness" and alert intervention teams.
- Sleep and Movement Correlation: By syncing with Apple Health or Fitbit data, the AI identifies how physical inactivity and poor sleep quality are directly impacting a user's daily mood.
- Early Warning Alerts: The system can send "nudge" notifications to the user or their doctor, suggesting a preemptive therapy session or a change in medication before a crisis hits.
- Longitudinal Data Tracking: This allows US clinics to see a "high-definition" view of a patient’s life between appointments, rather than relying on the patient’s memory of the past month.
Why it matters:
Early intervention is the "holy grail" of mental health care. By using predictive analytics, US healthcare systems can move from "disaster management" to "preventative maintenance," significantly reducing the number of emergency room visits and tragic outcomes.
3. Voice and Facial Expression Biomarker Analysis
AI in 2026 can "hear" and "see" things that the human ear and eye might miss. During teletherapy sessions, AI tools analyze vocal tones, speech speed, and micro-expressions to give therapists a deeper understanding of a patient's true emotional state. This technology is particularly useful in the USA for remote care, where a therapist might not be able to feel the "energy" of the room through a screen.
- Vocal Affect Recognition: The AI detects "flat affect" or tremors in the voice that are clinically associated with conditions like major depressive disorder or Parkinson’s-related anxiety.
- Micro-Expression Mapping: Using computer vision, the tool identifies brief flashes of fear, sadness, or anger that occur for just a fraction of a second during a conversation.
- Linguistic Sentiment Scoring: AI analyzes the specific choice of words to determine if a patient is moving toward "absolute" thinking, which is a common trait in severe anxiety.
- Real-Time Therapist Feedback: While a session is happening, the AI can provide a "dashboard" for the doctor, highlighting when the patient’s stress levels spiked during certain topics.
- Objective Documentation: The AI automatically generates a report of the emotional highs and lows of a session, making clinical note-taking faster and more accurate for US practitioners.
Why it matters:
This technology provides an objective layer to a traditionally subjective field. It helps US therapists make more data-driven diagnoses and ensures that subtle signs of distress are caught early, even in a virtual environment.
4. AI-Enhanced Personalized Medication Management
Finding the right psychiatric medication in the USA has historically been a process of "trial and error," which can be exhausting for patients. In 2026, AI will be used to analyze genetic data, previous treatment history, and real-time symptom tracking to predict which medication and at what dosage is most likely to work for a specific individual.
- Pharmacogenomic Integration: AI cross-references a user’s DNA markers with a vast database of drug interactions to find the best match for their unique biology.
- Side-Effect Prediction: The system monitors early physiological data from wearables to detect if a patient is experiencing negative side effects before they become severe.
- Dynamic Dosage Optimization: Instead of waiting for a monthly check-up, AI-driven apps can help doctors adjust dosages based on daily mood and biometric data.
- Adherence Reminders: Intelligent chatbots send personalized "smart reminders" that explain the importance of the medication, rather than just buzzing the phone.
- Drug Discovery Acceleration: Researchers in the US are using AI 3D models to screen new compounds for depression and anxiety, significantly speeding up the FDA approval process.
Why it matters:
Reducing the "trial and error" phase of medication saves months of suffering for patients. In the US, where healthcare costs are a major concern, this efficiency also reduces the financial burden of ineffective treatments and follow-up appointments.
5. Ambient Listening for Clinical Burnout Reduction
The administrative burden on US mental health professionals is a leading cause of burnout. In 2026, "ambient listening" AI tools will become standard in clinics. These tools sit in the room (or join the video call) and automatically transcribe the session, summarize the key themes, and update the Electronic Health Record (EHR) so the doctor can focus entirely on the patient.
- Automated SOAP Notes: The AI identifies the Subjective, Objective, Assessment, and Plan portions of the conversation and drafts a professional clinical note instantly.
- Action Item Extraction: It automatically pulls out "homework" or follow-up tasks discussed during the session and sends them to the patient’s app.
- Insurance Authorization Support: The AI can summarize the necessity of care in a way that aligns with insurance requirements, speeding up the claims process.
- Multi-Speaker Identification: Advanced microphones and software can distinguish between multiple family members in a session, accurately attributing quotes to each person.
- Privacy-First Processing: These tools are built with strict HIPAA-compliant encryption, ensuring that the session is processed locally and never stored in a way that identifies the patient.
Why it matters:
By removing the "paperwork tax," US therapists can see more patients and provide higher-quality, more focused care. This is a critical tool for retaining the current workforce and making the mental health profession sustainable for the future.
6. VR-AI Hybrid Exposure Therapy
For US veterans and individuals with PTSD or phobias, 2026 has brought the perfection of VR-AI hybrid therapy. Using Virtual Reality, patients are placed in controlled environments where they can face their fears. AI controls the intensity of the environment in real-time, responding to the patient's heart rate and stress levels to ensure the exposure is therapeutic and not re-traumatizing.
- Adaptive Environments: If a patient's heart rate gets too high, the AI "softens" the VR scenario perhaps by brightening the lights or slowing down the movement to keep them in the "growth zone."
- Simulated Social Interactions: For social anxiety, AI avatars can simulate various social scenarios, from a job interview to a first date, providing realistic and varied practice.
- PTSD Scenario Recreation: Veterans can work through specific traumatic memories in a safe, guided VR space that is precisely calibrated to their current level of resilience.
- Biofeedback Loops: The VR headset and wearable sensors create a closed loop where the AI constantly adjusts the experience based on the patient's physical response.
- Gamified Habit Building: For younger US patients, these VR experiences are often designed with game-like rewards to encourage consistency and engagement with the treatment plan.
Why it matters:
This use case takes the "fear" out of exposure therapy. By making the process highly controlled and personalized, it increases the success rate for treating some of the most difficult mental health conditions facing Americans today.
7. AI-Driven Workplace Wellness & Productivity
In the US corporate world of 2026, mental health is treated as a core business metric. AI tools are now integrated into workplace platforms like Slack or Microsoft Teams to monitor the collective "sentiment" of a team. They provide early warnings to managers about burnout trends and offer individual employees personalized "micro-interventions" to manage stress throughout the workday.
- Burnout Trend Analysis: The AI can flag when a team's communication style shifts toward "exhaustion" markers, allowing companies to implement "No-Meeting Fridays" or extra rest days.
- Personalized Stress Nudges: If the AI detects a high-stress day based on a packed calendar and rapid-fire messaging, it might suggest a 2-minute guided meditation.
- Employee Sentiment Surveys: AI can analyze anonymous feedback to give leadership an honest view of company culture and mental well-being without compromising individual privacy.
- Financial Stress Tools: Newer US-based platforms like Brightn combine mental wellness with financial planning AI, recognizing that money is a primary driver of anxiety for American workers.
- Skill-Matching for Fulfillment: AI helps employees find internal projects that align with their personal strengths and passions, reducing the feeling of "stagnation" and "quiet quitting."
Why it matters:
Workplace stress costs the US economy billions in lost productivity. By integrating AI wellness into the workday, companies can create a more supportive culture that values human capital as much as financial capital.
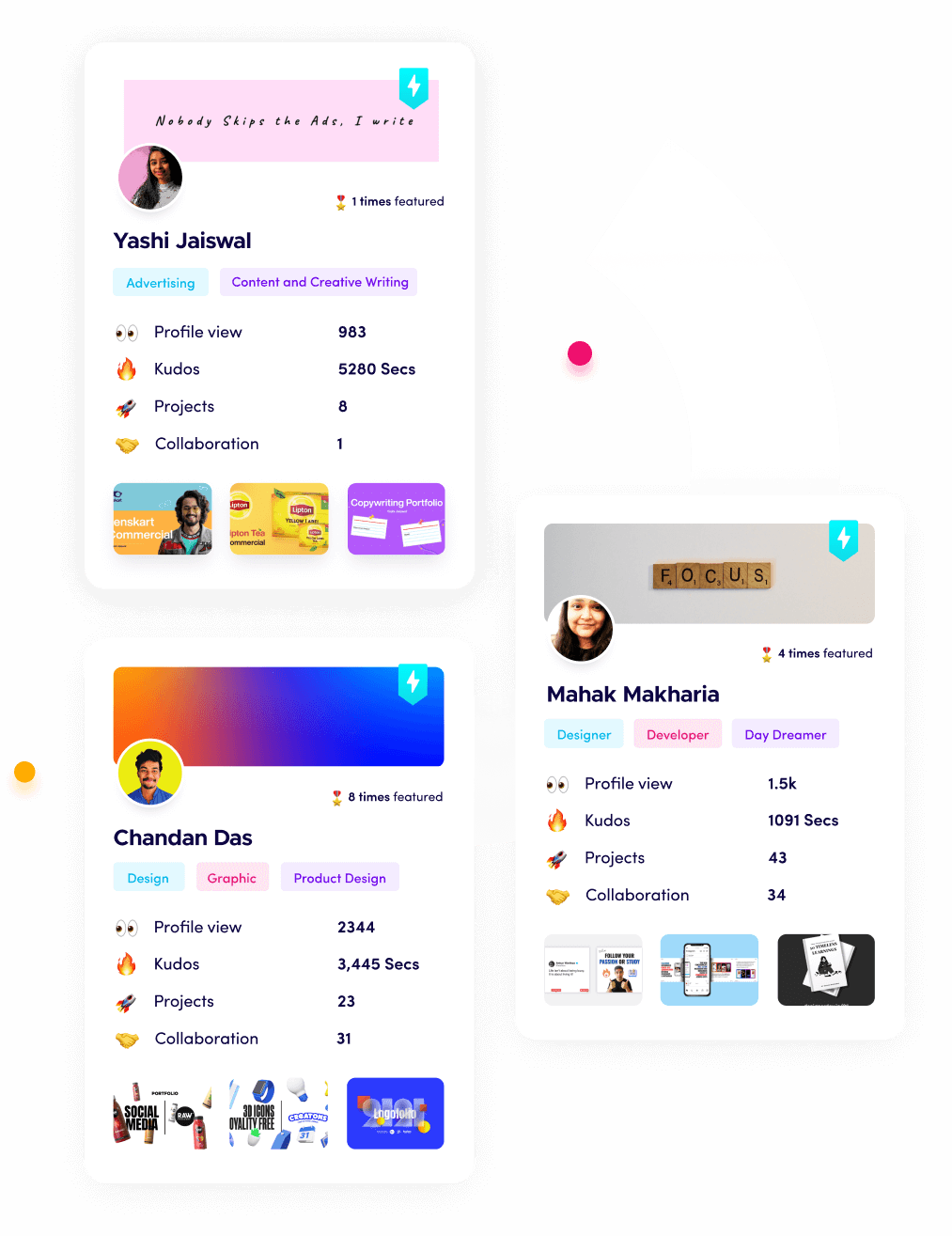
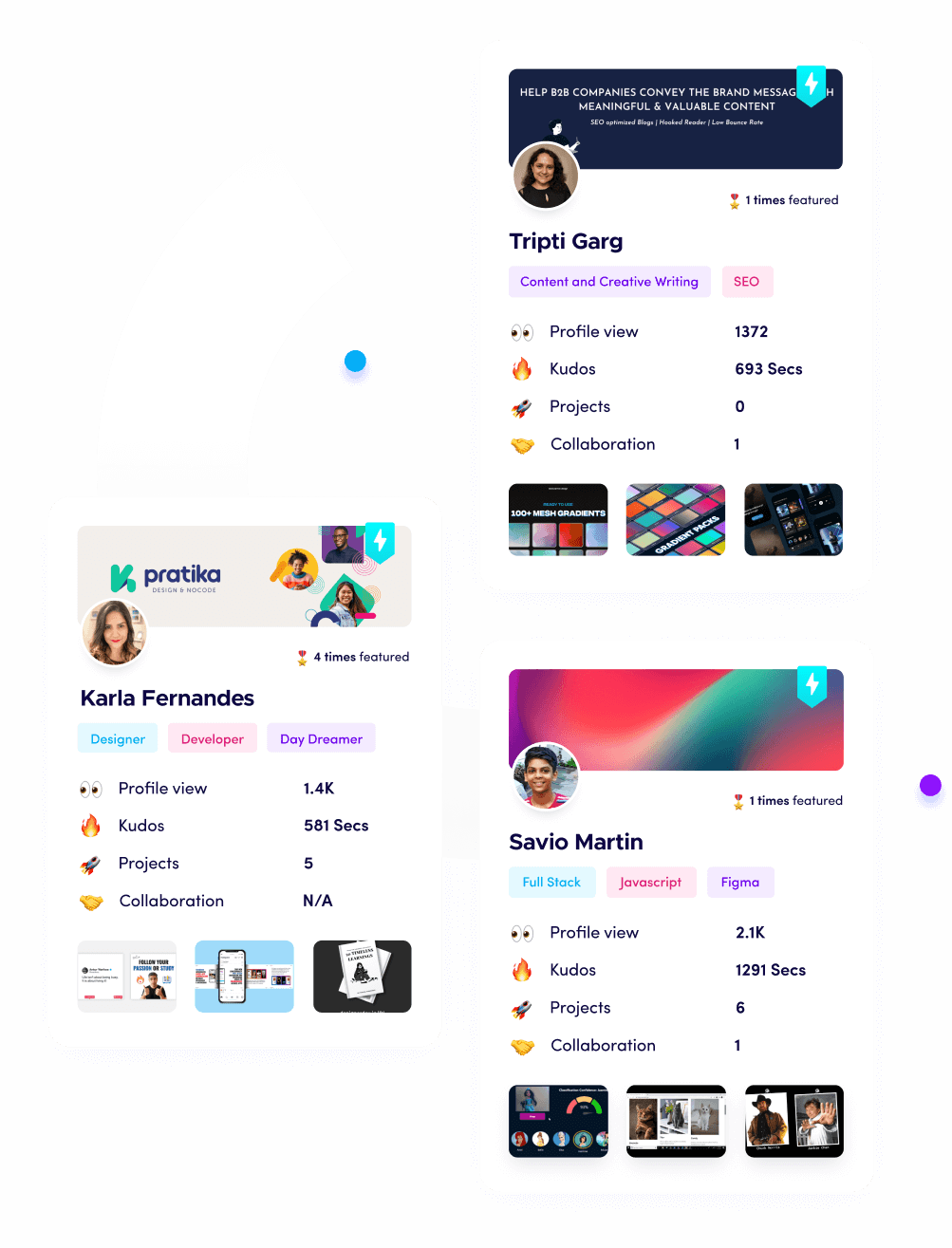
Showcasing Your Skills with Fueler
As the mental health tech industry grows in the USA, the demand for talented developers, designers, and researchers is at an all-time high. This is where Fueler becomes your most valuable asset. Instead of a boring, traditional resume, Fueler allows you to showcase your "proof of work" in this specialized field. Whether you have designed a new AI chatbot interface or written the code for a predictive algorithm, Fueler helps you organize these projects into a professional portfolio that speaks directly to high-ticket health-tech companies.
Fueler Pricing:
- Fueler Premium: $96 per year (approx. 8,000 INR per year)
Final Thoughts
The rise of AI in US mental health care is not about removing the human touch, it is about magnifying it. In 2026, we are seeing a shift where technology handles the data, the tracking, and the 24/7 availability, so that human clinicians can focus on what they do best: deep connection and complex healing. As these tools become more affordable and accurate, the goal of "mental health for all" in the USA is finally moving from a dream to a reality. The future of wellness is intelligent, personalized, and, most importantly, accessible to everyone.
FAQs
Are AI mental health tools HIPAA compliant in the USA?
Yes, most reputable AI platforms used in clinical settings in 2026 are built with strict HIPAA-compliant encryption to ensure that sensitive patient data is protected. Always check the privacy policy of any app to see how your data is stored and who has access to it before sharing personal information.
Can an AI chatbot replace my real therapist?
While AI chatbots are excellent for 24/7 support, mood tracking, and practicing CBT skills, they are not designed to replace licensed human therapists. In 2026, the best approach is "blended therapy," where you use AI tools between your regular sessions with a human professional for the best results.
How much do AI mental health apps cost for US users?
Prices vary depending on the level of support. Simple AI chatbots and meditation apps often have free tiers, while premium versions with advanced tracking or live coaching typically range from $10 to $75 per year. Some "prescription-only" AI digital therapeutics may even be covered by US health insurance plans.
Is AI mental health technology safe for children and teens?
Many AI wellness tools are designed specifically for younger audiences with extra safety guardrails. However, parents should look for apps that are clinically validated and have "human-in-the-loop" systems that can alert a guardian or a professional if the AI detects signs of a serious crisis.
Can AI detect depression just from my voice?
In 2026, yes. Advanced "voice biomarker" technology can analyze hundreds of subtle vocal features like pitch, rhythm, and breathiness to identify patterns that are statistically linked to depression. This is often used as a screening tool to help people realize they might need to seek professional help.
What is Fueler Portfolio?
Fueler is a career portfolio platform that helps companies find the best talent for their organization based on their proof of work. You can create your portfolio on Fueler. Thousands of freelancers around the world use Fueler to create their professional-looking portfolios and become financially independent. Discover inspiration for your portfolio
Sign up for free on Fueler or get in touch to learn more.