Top 7 AI Use Cases in Mental Health Across Europe (2026)

Riten Debnath
21 Jan, 2026

The European mental healthcare landscape is currently undergoing a radical structural shift. With a growing professional shortage across the continent, from Berlin to Budapest, clinicians are increasingly turning to machine learning and natural language processing to bridge the gap between patient needs and provider availability. Unlike the experimental phase of previous years, the current environment is defined by "Agentic AI" acting as an operational layer within healthcare systems. These systems don't just provide insights; they coordinate care, automate administrative burdens, and offer personalized interventions that adhere to the stringent requirements of the EU AI Act, ensuring that innovation remains both ethical and patient-centric.
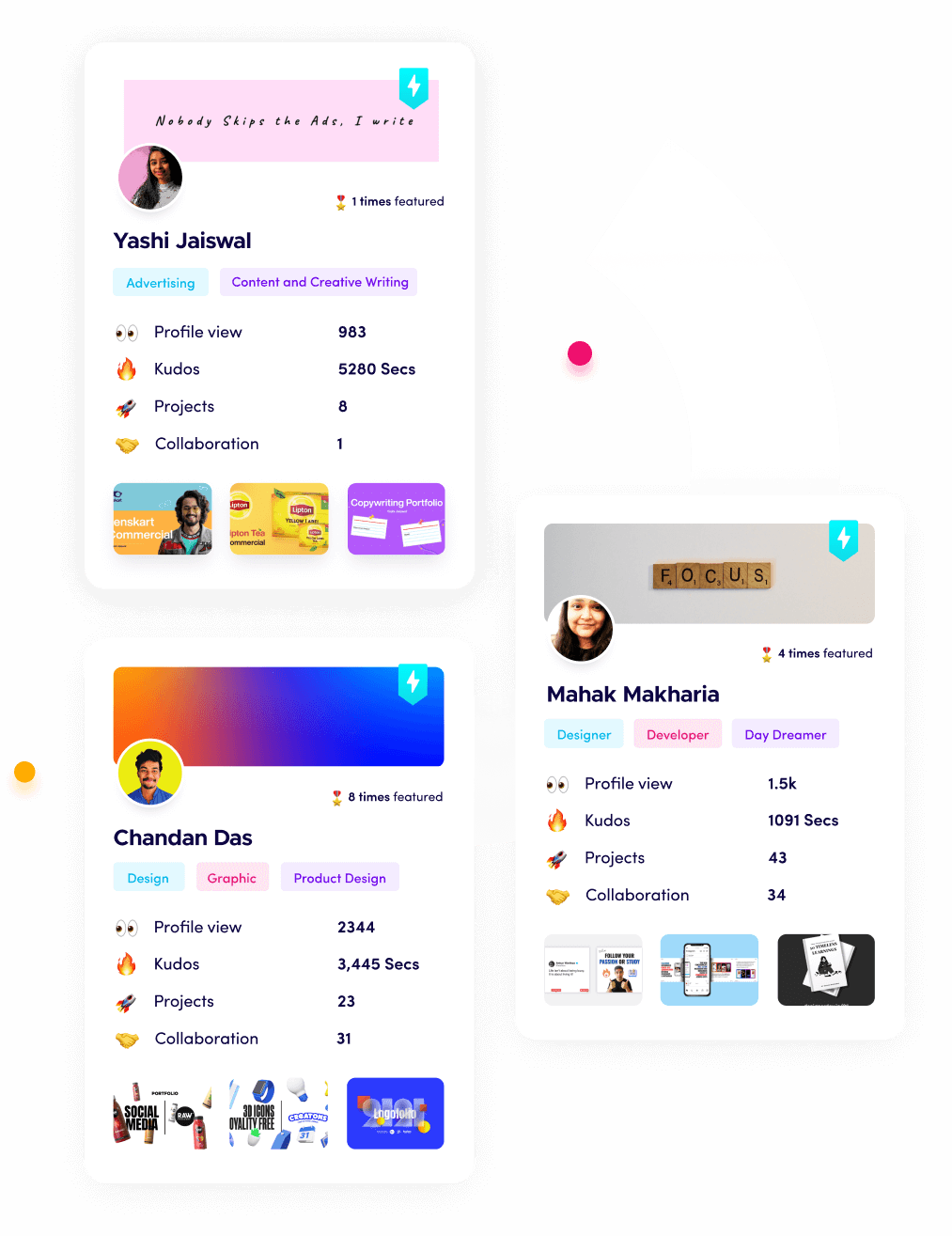
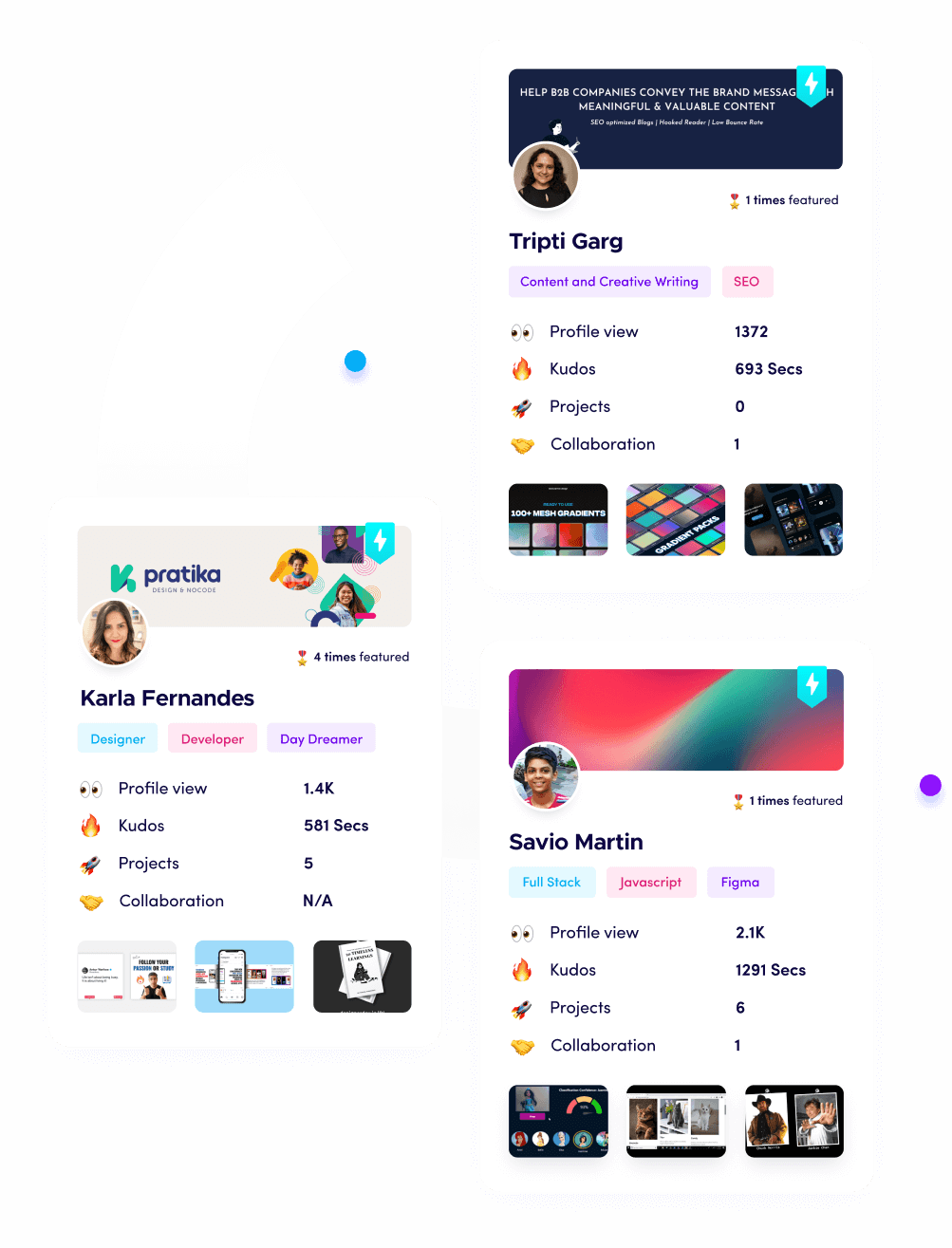
I’m Riten, founder of Fueler, a skills-first portfolio platform that connects talented individuals with companies through assignments, portfolios, and projects, not just resumes/CVs. Think Dribbble/Behance for work samples + AngelList for hiring infrastructure
Precision Diagnostics and Operational Intelligence
1. Digital Phenotyping and Early Warning Systems
Digital phenotyping involves the real-time collection of "passive" data from smartphones and wearables to create a high-resolution map of a patient's mental state. AI algorithms analyze typing speed, sleep disturbances, and social interaction patterns to detect the subtle "prodromal" signs of a manic episode or a depressive relapse long before the patient becomes symptomatic. In European clinical settings, this allows for a move from reactive treatment to proactive prevention, where care teams receive automated alerts to intervene during high-risk windows, effectively reducing emergency hospitalizations and long-term disability.
- Non-Intrusive Behavioral Monitoring: By leveraging the accelerometers and usage sensors already present in modern smartphones, AI can identify shifts in physical activity or communication frequency that statistically correlate with worsening mental health states.
- Proactive Crisis Intervention: When data patterns suggest an imminent crisis, systems can automatically trigger "Just-in-Time" interventions, such as pushing breathing exercises to a patient's device or notifying a designated crisis counselor in real-time.
- Objective Longitudinal Data Sets: This technology provides clinicians with an objective record of a patient's behavior between appointments, removing the "recall bias" that often hampers accurate diagnosis during standard face-to-face consultations. For an online psychiartist, this kind of longitudinal behavioral signal becomes structurally important, as treatment decisions are often made without the benefit of in-room observation, informal affect cues, or third-party collateral input
- Privacy-First Data Processing: To comply with the latest European data standards, these systems typically use "on-device" processing, ensuring that sensitive behavioral data never leaves the user's phone without explicit, granular consent.
- Specific Disorder Mapping: Current research across the EU is focusing on developing specific digital biomarkers for complex conditions like schizophrenia and bipolar disorder, where early detection is critical for managing long-term outcomes.
Price Point: Enterprise licenses for health systems typically range from €10,000 to €50,000 annually, while consumer-facing apps like Headspace (formerly Ginger) offer tiered corporate pricing based on headcount.
2. Ambient AI Scribes and Administrative Automation
The administrative burden on European psychiatrists and nurses has reached a tipping point, but "Ambient Clinical Intelligence" is now being used to reclaim hours of lost time every day. These AI systems "listen" to therapy sessions with consent and automatically generate structured clinical notes, such as SOAP or GIRP reports, allowing the provider to focus entirely on the patient rather than a screen. By integrating directly into European Electronic Health Records (EHR) and automating billing codes, these tools are significantly reducing clinician burnout and increasing the capacity of mental health clinics to see more patients.
- Real-Time Natural Language Processing: The AI identifies key clinical themes, medication mentions, and risk factors during a conversation, distilling an hour-long session into a concise, accurate medical record in seconds.
- Burnout Reduction for Providers: Studies show that automated documentation can save clinicians up to three hours of paperwork per day, allowing them to reinvest that time into direct patient care or personal well-being.
- Accuracy and Compliance Audits: These tools don't just write; they audit the path to a clinical decision, ensuring that all notes meet the transparency requirements of the EU AI Act and national health insurance standards.
- Interoperability with Local EHRs: Leading European providers are prioritizing tools that sync flawlessly with existing hospital IT infrastructure, moving away from fragmented point solutions that create data silos.
- Multilingual Capacity for EU Markets: Modern scribes are being trained to handle the diverse linguistic landscape of Europe, accurately capturing sessions in French, German, Spanish, and English while maintaining clinical nuance.
Price Point: Professional tools like Wolters Kluwer's ambient solutions or Heidi Health typically cost between €30 and €100 per clinician per month, depending on the volume of sessions and integration depth.
3. AI-Driven Triage and Intelligent Patient Intake
European health systems are shifting away from a "first-come, first-served" model to one driven by intelligent prioritization. AI-powered intake platforms can analyze a patient's history, recent emergency room visits, and self-reported symptoms to answer the critical question: "Given our current capacity, which patients have the most urgent need?" This "Intelligent Triage" ensures that limited clinical resources are allocated to those at the highest risk of crisis, significantly improving the efficiency of resource allocation across rural and urban mental health programs.
- Pattern Analysis in Utilization Data: The system identifies individuals who are frequent "no-shows" or have increasing Emergency Department visits, flagging them as high-acuity cases that require more immediate clinical attention.
- Probability Engines for Risk Assessment: By analyzing unstructured data from intake forms, the AI calculates the statistical probability of self-harm or escalation, allowing clinics to prioritize crisis cases over routine appointments.
- Automated Scheduling Optimization: AI models can predict which patients are most likely to miss an appointment and overbook or fill those slots in real-time, ensuring that clinical staff time is never wasted.
- Closing Gaps in Care Management: Instead of just flagging a risk, these systems coordinate tasks across clinicians and payers to ensure that follow-up care is scheduled and completed within the required medical window.
- Democratizing Access to Triage: Digital intake tools provide a lower barrier to entry for patients who may be hesitant to speak to a person initially, allowing them to start the care process through a secure, non-judgmental interface.
Price Point: Integration of AI triage models into existing health system software often requires custom enterprise pricing, generally starting at €25,000 per year for medium-sized clinical networks.
4. Vocal Biomarkers for Depression and Anxiety Screening
The way we speakour pitch, tone, and rhythmholds "acoustic biomarkers" that are often invisible to the human ear but detectable by high-frequency AI analysis. European researchers are increasingly using these vocal biomarkers as objective screening tools for major depressive disorder (MDD) and post-traumatic stress disorder (PTSD). By integrating these algorithms into telehealth platforms or even standard telephone screening, providers can identify emotional changes and symptom severity with a level of accuracy that complements traditional psychiatric assessments.
- Analysis of Acoustic Fluctuations: AI models look for "prosodic" features, such as increased pauses, flattened pitch, or changes in speech rate, which are known clinical indicators of psychological distress.
- Scalable Population Screening: Because these tools only require a short audio sample, they can be deployed at scale to screen large populations, flagging high-risk individuals for further clinical evaluation.
- Objective Severity Tracking: As a patient moves through treatment, vocal analysis provides an objective way to track progress, helping clinicians adjust medication or therapy based on tangible shifts in the patient's vocal profile.
- Remote Monitoring via Video Consultations: Telehealth providers are embedding these tools into video calls, giving psychiatrists real-time "emotional intelligence" dashboards that highlight subtle cues they might otherwise miss.
- Cross-Language Sentiment Analysis: Modern vocal AI is being trained to recognize emotional markers across different European languages, ensuring that the "sound" of depression is captured regardless of the specific dialect spoken.
Price Point: Specialty developers like Sonde Health or Cogito provide API-based pricing for health platforms, often ranging from €1 to €5 per screened user per month.
5. VR Exposure Therapy with Real-Time Biofeedback
Virtual Reality (VR) combined with AI is revolutionizing how phobias and PTSD are treated in European specialized clinics. These systems create immersive environments that "adapt" in real-time to the patient's physiological state. If a patient's heart rate or skin conductance indicates they are becoming overwhelmed, the AI dynamically softens the stimuli to keep the therapy challenging but safe. This "closed-loop" feedback system ensures that exposure therapy is precisely calibrated to the individual’s tolerance levels, leading to faster recovery times.
- Dynamic Stimuli Adjustment: The AI engine monitors biofeedback and modifies the intensity of the VR scenario, such as the number of "triggers" present, to maintain the patient within their optimal "therapeutic window."
- Safe and Controlled Environments: VR allows patients to confront their fears (like social anxiety or specific phobias) in a setting where the clinician has total control, removing the unpredictability and risk of real-world exposure.
- Immersive Narrative Development: AI can generate personalized scenarios based on a patient's specific trauma or history, making the therapy significantly more relevant and impactful than generic "out-of-the-box" VR programs.
- Data-Validated Progress Tracking: Every session generates a detailed report of the patient's physiological reactions, providing clear data on their desensitization progress over multiple weeks of treatment.
- Accessible Specialized Care: High-end VR systems are being deployed to smaller clinics across Europe, giving patients in remote areas access to the same quality of specialized PTSD treatment as those in major medical hubs.
Price Point: Professional VR headsets paired with clinical software like Virtually Better or Pious typically cost around €2,500 for the hardware and €150–€300 monthly for the therapeutic software license.
6. Pharmacogenomics and Precision Medication Management
One of the most frustrating aspects of mental health treatment is the "trial and error" period for finding the right antidepressant or antipsychotic. AI is solving this by analyzing a patient's genetic markers alongside their medical history and lifestyle data to predict which medications are most likely to be effective. This precision medicine approach, increasingly common in leading European hospitals, shortens the time to recovery and significantly reduces the risk of adverse side effects that can lead to patients discontinuing their treatment.
- Genetic Predictors of Drug Efficacy: AI models cross-reference a patient's DNA with massive databases of clinical outcomes to determine how their body is likely to metabolize specific psychiatric medications.
- Reduction of Adverse Effects: By identifying medications that a patient is genetically predisposed to react poorly to, clinicians can avoid "toxic" prescriptions, improving patient safety and treatment adherence.
- Personalized Dosage Recommendations: Beyond just choosing the drug, AI helps determine the optimal starting dose based on a patient's unique biological profile, further refining the "precision" of the intervention.
- Integration of Social Determinants: Advanced models are beginning to include lifestyle such as diet and sleep into the prediction engine, acknowledging that biology is only one part of the medication success equation.
- Long-Term Treatment Optimization: As a patient’s health data grows, the AI continues to refine its recommendations, helping clinicians manage long-term medication changes with much higher confidence.
Price Point: Individual pharmacogenomic tests in Europe (like GeneSight equivalents) typically cost between €300 and €600 per test, with the AI analysis included in the lab fee.
7. Conversational CBT and Agentic Support Bots
The most visible application of AI in mental health is the high-level conversational agent trained in Cognitive Behavioral Therapy (CBT). Unlike the basic chatbots of the past, these 2026-era "Agentic Support" bots use Large Multi-Modal Models to engage in deep, empathetic dialogue. They are increasingly being used as "Digital Therapeutics" that patients can access 24/7 to practice coping skills, challenge negative thought patterns, and manage anxiety between their weekly human therapy sessions.
- Structured CBT Interventions: These bots guide users through clinically validated exercises, helping them recognize cognitive distortions and build resilience through interactive, text-based or voice-based modules.
- 2026-Era Crisis Escalation: Advanced natural language understanding allows these bots to detect keywords or "sentiments" related to self-harm, instantly bridging the user to a human crisis line or emergency services.
- High-Frequency Emotional Support: For patients who feel isolated or geographically remote, these bots provide a persistent, non-judgmental presence that offers instant support during the "quiet hours" when traditional clinics are closed.
- Anonymity and Reduced Stigma: Many users feel more comfortable sharing their initial symptoms with an AI than with a person, making these bots an essential "entry point" into the broader European mental healthcare system.
- Clinical Adherence Monitoring: The bot can track how often a patient is practicing their therapeutic "homework" and share that data (with consent) with their primary therapist to improve the effectiveness of in-person sessions.
Price Point: Many apps are free for basic tiers, while "Premium" therapeutic versions (prescribed by doctors) are often reimbursed by national health systems in countries like Germany and the UK.
Build Your Professional Impact with Fueler
As the mental health sector integrates these advanced AI tools, the demand for professionals who understand the intersection of "Care and Code" is skyrocketing. Whether you are a clinician implementing these tools or a developer building them, you need a way to showcase your expertise. Fueler is the leading platform for documenting your "Proof of Work" in the healthcare tech space. By creating a Fueler portfolio, you can highlight your successful AI implementations, research papers, and collaborative projects, positioning yourself as a leader in the next generation of European mental healthcare.
Final Thoughts
The integration of AI into European mental health is no longer about "replacing" clinicians; it is about empowering them. The top use cases today focus on operational efficiency, precision, and early intervention, three areas where human resources are most strained. As we move further into this new era of care, the successful organizations will be those that prioritize "Trust and Transparency" as much as technical capability. By leveraging these seven AI use cases, the European mental health system is not just becoming more efficient it is becoming more human by giving providers the time and data they need to truly care.
FAQs
Are AI therapists a replacement for human psychologists?
In the current European medical landscape, AI is viewed as an adjunct, not a replacement. AI tools are excellent for administrative tasks, screening, and providing 24/7 "coping skill" support, but they lack the complex emotional depth and "therapeutic alliance" that is critical for treating severe psychological trauma and complex mental illnesses.
How does the EU AI Act affect mental health apps?
The EU AI Act categorizes most AI tools in healthcare as "High-Risk." This means that mental health apps and diagnostic tools must meet strict requirements for documentation, transparency, and human oversight. This regulation is designed to protect European citizens from "algorithmic bias" and ensure that any AI-driven diagnosis is safe and reliable.
Can AI predict suicide or self-harm accurately?
While AI is remarkably good at "pattern recognition" and identifying high-risk individuals through clinical data and social signals, it is not a "crystal ball." It is used to flag patients for human intervention, allowing clinicians to prioritize their time toward those who the data suggests are in the greatest need of immediate care.
How is my data protected when using an AI mental health tool?
Under GDPR and the latest 2026 privacy standards, European mental health data is subject to "special category" protections. Most reputable tools now use end-to-end encryption and often process sensitive data "locally" on your device, ensuring that your most personal thoughts and behaviors are never shared or stored in a way that could compromise your privacy.
Why is Germany leading in "Digital Health Applications" (DiGA)?
Germany was one of the first countries in Europe to create a clear legal pathway for doctors to "prescribe" digital health apps. This has led to a booming ecosystem of clinically validated mental health tools that are fully reimbursed by statutory health insurance, making high-quality AI support accessible to millions of German citizens.
What is Fueler Portfolio?
Fueler is a career portfolio platform that helps companies find the best talent for their organization based on their proof of work. You can create your portfolio on Fueler. Thousands of freelancers around the world use Fueler to create their professional-looking portfolios and become financially independent. Discover inspiration for your portfolio
Sign up for free on Fueler or get in touch to learn more.