Optimizing Packaged Software for US Healthcare Platforms

Riten Debnath
26 Aug, 2025

Healthcare technology in the US is experiencing fast-paced change, with packaged software needing to keep up with shifting compliance, interoperability, and patient experience demands. Hospitals, clinics, and health tech startups all face the challenge of getting more from their software investments balancing HIPAA, user-friendliness, and real-time integrations without breaking the bank or risking patient safety.
I’m Riten, founder of Fueler, a platform that helps professionals get hired by showing real work samples. Just as a strong portfolio is proof of your skills and reliability, optimizing your healthcare platform’s packaged software demonstrates operational strength and trustworthiness to patients, partners, and regulators. In this article, I break down the most actionable and up-to-date strategies to upgrade, integrate, and maximize packaged health IT solutions for the US market.
Why Is Packaged Software Optimization Important in US Healthcare?
Packaged health IT (Electronic Health Records, telehealth apps, billing solutions, and more) delivers the basic infrastructure for modern care. But US healthcare organizations compete in a landscape defined by tight margins, complex privacy laws, and high patient expectations making it essential to get more out of every deployed tool.
- EHR, billing, scheduling, and patient portals must all communicate seamlessly.
- HIPAA enforcement and state regulations set the bar for privacy and security.
- Performance impacts patient outcomes, satisfaction, and business viability.
- Rapid advances in telehealth and data exchange challenge legacy systems.
Why it matters: Optimizing packaged solutions isn’t just about speed or convenience it’s about compliance, competitive advantage, and building patient trust in every digital interaction.
Key Strategies for Optimizing Packaged Software in US Healthcare
1. Prioritize Interoperability and Open Standards
Ensuring that different software tools share data accurately is a cornerstone of digital health success. Embracing open standards like HL7 FHIR and adopting APIs lets different platforms (EHR, labs, imaging, billing) talk to each other without costly data translation.
- Choose software known for strong API/HL7 support.
- Demand seamless integration with labs, pharmacies, insurers, and patient apps.
- Insist on robust data mapping and exchange protocols.
- Work with vendors that participate in Carequality and CommonWell networks.
Why it matters: Siloed data leads to duplicate work, medical errors, and poor patient experiences. Interoperable systems drive efficient care, lower costs, and compliance with US rules.
2. Maximize Security and HIPAA Compliance
Protecting patient data is legally required and non-negotiable in the US. Packaged solutions must enable easy encryption, tight access controls, and detailed audit trails not just “tick the box” certifications.
- Seek tools with strong end-to-end encryption, not just “at rest.”
- Regularly update software to address new vulnerabilities.
- Monitor user access with customizable permissions and active session logs.
- Use automated compliance reporting for HIPAA and HITECH.
Why it matters: Optimizing security minimizes regulatory risk, avoids costly breaches, and assures patients that their data is safe in the connected world of digital health.
3. Streamline User Experience (UX) for Clinical and Administrative Staff
Even advanced tools fail if users find them clunky or slow. US clinicians and staff are under time pressure intuitive workflows, shortcut features, and responsive support are essential.
- Implement role-based dashboards that display relevant data only.
- Customize workflows to fit common clinical or billing scenarios.
- Offer in-app guidance, AI-powered suggestions, and fast support resources.
- Continuous UX feedback loops with real frontline users.
Why it matters: Smooth user experience reduces errors, increases adoption rates, and lifts job satisfaction, which means better patient outcomes and fewer operational headaches.
4. Harness Analytics and Reporting to Drive Care Improvements
Healthcare providers need actionable insights to drive better outcomes and business decisions. The best-optimized packaged solutions go beyond static charts to provide advanced, customizable analytics.
- Deploy real-time dashboards for clinical KPIs and financial health.
- Enable easy exports for payor reporting and quality initiatives.
- Integrate with AI tools for predictive analytics and population health.
- Ensure compliance-focused reporting (MIPS, MACRA, value-based care).
Why it matters: Powerful analytics transform vast healthcare data into evidence-backed decisions, helping both care teams and executives meet US performance standards.
5. Integrate with Telehealth and Patient Engagement Platforms
Telemedicine and digital engagement are exploding in the US, especially post-pandemic. Optimized packaged solutions need to connect directly to video visits, secure messaging, and online appointment tools.
- Support for HIPAA-compliant video and chat built-in or easy to add-on.
- Patient portals for self-scheduling, record access, and payments.
- Automated appointment reminders and follow-up systems.
- Mobile-first design for both clinicians and patients.
Why it matters: Integrated telehealth and engagement features enhance patient access, boost satisfaction, and help providers stay competitive in an increasingly digital marketplace.
6. Enable Scalability and Modular Upgrades
US health organizations grow and change quickly. Your software needs to keep pace. Modularity ensures you can add new service lines, users, or compliance fixes without a full system reboot.
- Use vendors offering modular upgrades and pay-as-you-grow licensing.
- Look for cloud-based solutions that support easy scaling.
- Simplify onboarding for new sites, specialties, or remote teams.
- Strong migration and support options for painless future updates.
Why it matters: Scalable software investments protect your organization from vendor lock-in and expensive, disruptive system changes.
7. Leverage RPA (Robotic Process Automation) and AI to Eliminate Repetitive Tasks
Implementing RPA and AI features in packaged healthcare platforms lightens the load of manual data entry, appointment reminders, claims tracking, and routine admin freeing up time for clinicians to focus on care.
- Automated extraction of data from faxes, scanned documents, or emails.
- Smart scheduling assistants and AI chatbots for patient support.
- Bots to streamline claims processing and revenue cycle management.
- Real-time error detection and workflow optimization through machine learning.
Why it matters: Embracing automation raises efficiency, reduces burnout, and lowers operational costs, offering a crucial edge in the rapidly evolving US health system.
Fueler — The Talent Bridge for Healthcare Tech
As US healthcare tech grows, finding professionals who can implement, optimize, and troubleshoot packaged solutions is both challenging and crucial. Fueler helps companies by letting them assess IT, integration, and data security expertise through job-sample assignments. This reduces hiring risks and ensures you bring in experts who can deliver real results — much as an optimized software portfolio proves system value, an optimized hiring process proves capability up front.
Final Thought
The future of US healthcare depends on how well organizations can optimize their packaged software. Focus on open interoperability, robust security, usability, analytics, and smart automation to ensure platforms do more than “check the box” — they truly enable better care, efficiency, and business growth. The right approach unlocks the full value of your digital infrastructure and keeps you ahead in an industry shaped by constant change.
Frequently Asked Questions (FAQs)
1. What are the key features to prioritize when selecting packaged software for US healthcare?
Look for strong interoperability, robust HIPAA security, user-friendly interfaces, support for analytics and reporting, scalable modules, and built-in telehealth capabilities.
2. How can clinics ensure compliance with US healthcare regulations when optimizing software?
Select vendors with proven HIPAA compliance, demand detailed audit trails, enable regular software updates, and provide staff compliance training.
3. Why is interoperability so important for US healthcare software?
Interoperability enables different systems (EHR, billing, imaging) to exchange data smoothly, improving care coordination, reducing errors, and meeting regulations like the 21st Century Cures Act.
4. Can small US healthcare providers benefit from software optimization?
Yes, even small practices gain efficiencies, better reporting, and higher patient satisfaction through scaled-down but optimized packaged tools tailored to their needs.
5. How do I find health IT professionals with real software optimization skills?
Fueler allows you to assess candidate expertise through hands-on assignments tailored to healthcare IT scenarios, helping ensure the right skills for your project.
What is Fueler Portfolio?
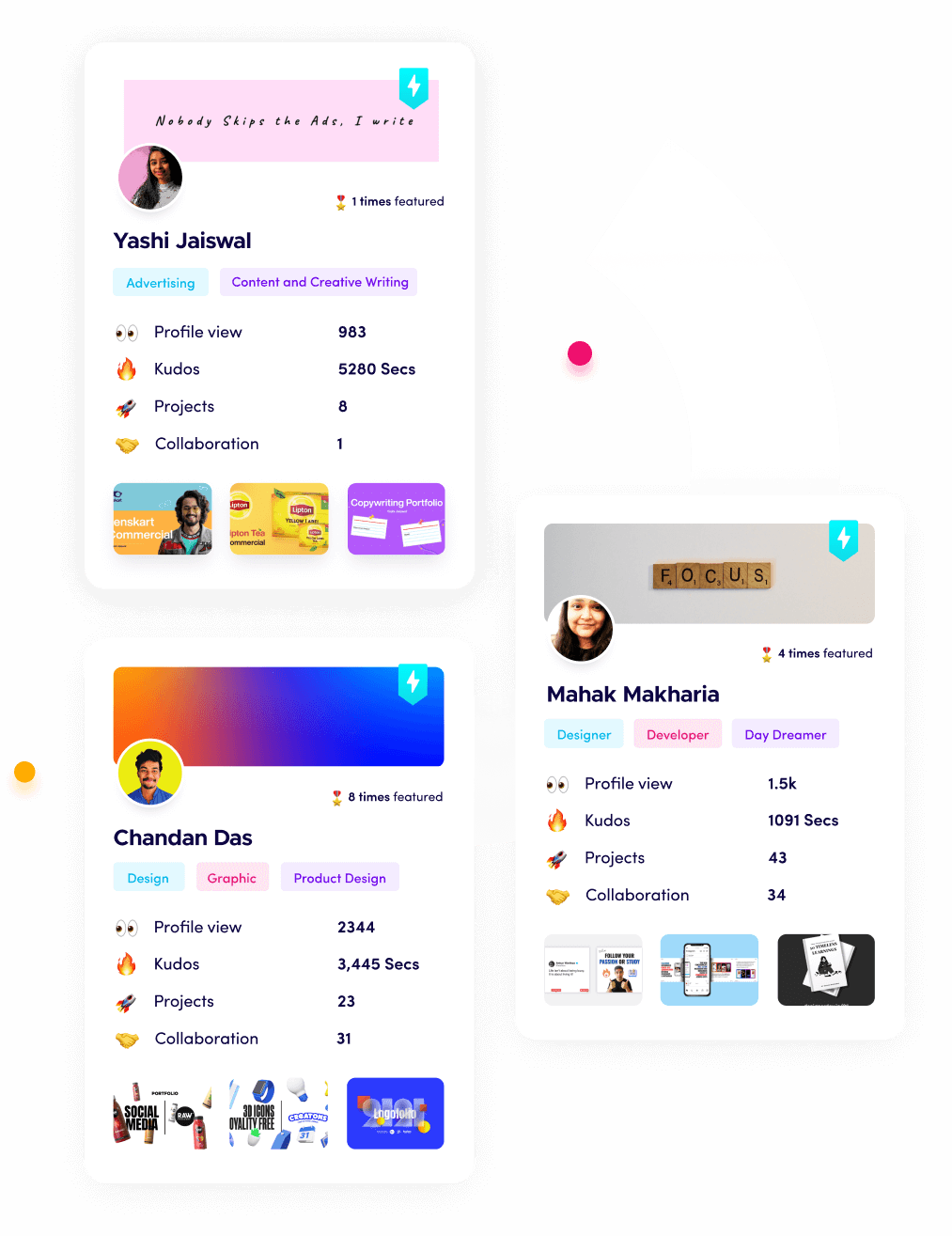
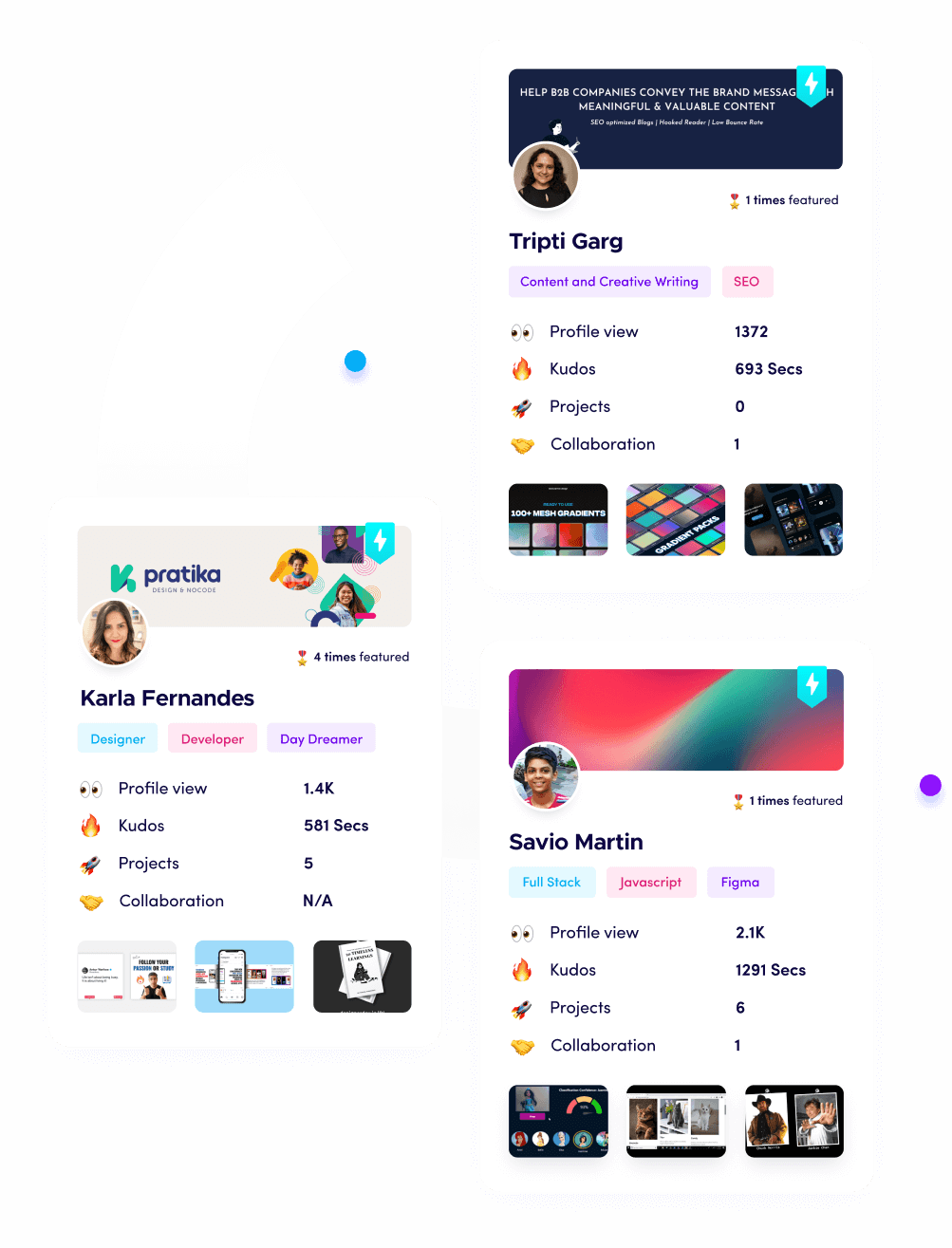
Fueler is a career portfolio platform that helps companies find the best talents for their organization based on their proof of work.
You can create your portfolio on Fueler, thousands of freelancers around the world use Fueler to create their professional-looking portfolios and become financially independent. Discover inspiration for your portfolio
Sign up for free on Fueler or get in touch to learn more.